Nirupama Saha
Department of Paediatric Surgery, Shaheed Suhrawardy Medical College and Hospital, Dhaka, Bangladesh.
Sajal Kumar Majumdar
Department of Paediatric Surgery, Shaheed Suhrawardy Medical College and Hospital, Dhaka, Bangladesh.
Mirza Kamrul Zahid
Department of Paediatric Surgery, Shaheed Suhrawardy Medical College and Hospital, Dhaka, Bangladesh.
Writtika Majumdar
Dhaka Medical College Hospital, Dhaka, Bangladesh.
Md Samsuzzaman Khan
Department of Paediatric Surgery, Shaheed Suhrawardy Medical College and Hospital, Dhaka, Bangladesh.
Abdullah Al-Mamun
Department of Paediatric Surgery, Shaheed Suhrawardy Medical College and Hospital, Dhaka, Bangladesh.
Rajib Dey Sarker
Department of Paediatric Surgery, Shaheed Suhrawardy Medical College and Hospital, Dhaka, Bangladesh.
Keywords: Cholecystitis, Paediatric population, Pathophysiologic pattern, Abdominal ultrasound.
DOI: 10.3329/bmrcb.v47i3.59244
Abstract
Background: In recent years, an increasing trend of paediatric cholecystitis is noticed in literature along with changing spectrum of biliary tract disease.
Objectives: The study was aimed to evaluate pediatric cholecystitis pointing on its underappreciated but important aetio-pathophysiological reasons and pattern.
Methods: This prospective type of observational study was done from November 2019 to April 2020 among a total of 65 children of acute and chronic cholecystitis (clinical manifestation not ≥72hours -acute; and for ≥6months with ≥3episodes-chronic). Data were collected on socio-demographic and clinical findings, laboratory results and image (abdominal ultrasound, and HIDA scan) findings, along with operative and histopathological (postoperative) findings.
Results: The mean age of the patients was 8.35 years, with male/female=1.17 and 48(73.8%) were from low socioeconomic condition. Preoperatively, 42 (64.6%) patients were presented with acute cholecystitis and 23 (53.6%) were with chronic cholecystitis with the commonest symptom of upper abdominal colicky pain 57 (87.6%.) and sign of right upper quadrant tenderness 65(100.0%) in both cases. On image findings, presence of pericholecystic fluid with biliary sludge was the major finding 27 (64.0%) and then gall stone 12 (29.0%) in acute cholecystitis whereas in chronic cholecystitis, the commonest finding was, fibrosis of gallbladder wall 12 (52.0%) and then gallstone 8 (35.0%). All patients were treated operatively(open cholecystectomy= 35 (22.8%), laparoscopic =30 (19.5%). Post-operatively, in acute cases, thickened gallbladder wall was the major finding 29 (69.0%), but in chronic cases, fibrosis of gallbladder wall was the commonest 13 (57.0%) finding. Total 37 (56.4%) patients among 65 had found an association between cholecystitis and prior infestation of diseases pathogens (typhoid enteritis 10 (15.4%) was the commonest).The type of infestation was not independent with the type of cholecystitis but a relationship between two was present (p=0.5671).
Conclusion: Acute acalculous cholecystitis with biliary sludge accounts for the majority of paediatric cholecystitis and there was an association between paediatric cholecystitis with prior infestation of disease pathogens.
Keywords: Cholecystitis, Paediatric population, Pathophysiologic pattern, Abdominal ultrasound.
Introduction
Cholecystitis, an inflammatory disease of the gallbladder, is relatively uncommon in children than adults, however, in recent years, an increasing trend of pediatric cholecystitis is noticed inliterature along with changing spectrum of biliary tract disease.1-4 Yet, most of the literature commonly emphasis on cholelithiasis owing to haemolytic disorders or biliary dyskinaesia rather focusing on the nature of the cholecystitis- acute or chronic.1,4-9 Again, clean cut diagnosis of paediatric (acute or chronic) cholecystitis with their pathological findings is often a challenge because of socio-demographic variances , the disease process or disease pathogenesis diversity, vague clinical manifestations and complex clinical situation.1,10-12,14-18 Sometimes, particularly, acute acalculou scholecystitis (ACC) is related to combination of multiple factors and it’s the pathogenesis is yet not clearly defined.19 Again, a relationship between prior infestation of disease pathogens is also observed in cholecystitis of paediatric population.11,20,21 However, still, maximum operations are with cholelithiasis oriented, so, there is paucity of data on pediatric cholecystitis particularly related to under-appreciated but significant reasons of the disease.22 Hence, the current study was aimed to evaluate the clinical and pathophysiological pattern of paediatric cholecystitis focusing on its undervalued but important reasons and predictors to ensure better patients’ outcome with decrease morbidity.
Materials and Methods
This observational study was carried out from November 2019-April 2020 among 65 eligible samples out of 97 admitted cases in the department of paediatric surgery Shaheed Suhrawardy Medical College Hospital, Dhaka with the clinical findings suggestive of an inflammatory biliary process either acute or chronic belonging to age group (2-14) years of both sexes. Patients without having any gross cardiac, renal, pulmonary or hepatic impairment, trauma or burn injury and with the preoperative clinical criteria of a possible inflammatory process with laboratory findings (an elevated white blood cell (WBC) count, CRP, serum bilirubin label, alkaline phosphatase label, and SGPT) or imaging and radiographic (ultrasound, CT, or HIDA) findings that indicated an inflammatory process were enrolled. Clinical manifestation ≥72 hours was considered as acute whereas manifestation lasting for more than 6 months with recurrent episodes (≥3 episodes) was taken into account as chronic. Fever from the medical notes, thickening of the gallbladder wall (≥4 mm) based on abdominal ultrasound, radiologic and /or sonological indications of acute inflammation included pericholecystic fluid or evidence of an impacted stone, presence of mucosal membrane sludge was considered. Patients underwent for HIDA scan with the findings of delayed visualisation of the gall bladder between 1-4 hours was considered as a reliable sign of chronic cholecystitis. All preoperative imaging and radiological findings were reviewed by both the department of radiology imaging and the pediatric surgery. Post-operative findings of biliary sludge/Gallstone/ thickening of gall bladder wall/ fibrosis of gall bladder or biliary dyskinaesia or other findings were correlated with histopathological report. All included patients were of surgically treated (both open and laparoscopically) and had postoperative histopathology reports for final diagnosis. Pathologic specimens with the findings of chronic inflammation such as gall bladder wall fibrosis and without signs of acute inflammatory changes like raised vascularity or presence of acute inflammatory cell microscopically were diagnosed as chronic cholecystitis. Individuals with congenital biliary tract abnormalities, underwent cholecystectomy for a non- inflammatory indication or as part of a more complicated procedure such as biliary atresia and liver transplant or to resect a choledochal cyst or any congenital abnormality of hepatobiliary tree were excluded from the study. Clinical information and laboratory data related to disease were considered. Data were analysed by standard statistical analysis SPSS version 17. The present study was approved by the Institutional Review Board of Shaheed Suhrawardy Medical College Hospital, Dhaka, Bangladesh and National Research Ethics Committee of Bangladesh Medical Research Council (BMRC).
Results
The demographic distribution of patients included in the average age range of the patients was (2-14) years with mean age 8.35± 1.27 and 35 (22.8%) were male and 30 (19.5%) were female (table I).
|
Demographic Distribution |
Results (N=65, No. in %) |
|
|---|---|---|
|
Age |
2-4 |
5(7.7%) |
|
(Years) |
4-6 |
8(12.3%) |
|
6-8 |
17(26.2%) |
|
|
8-10 |
13(20.0%) |
|
|
10-12 |
12(18.5%) |
|
|
12-14 |
10(15.4%) |
|
|
Mean ± SD |
|
8.35 ± 1.27 |
|
Sex |
Male |
35 (22.8%) |
|
Female |
30 (19.5%) |
|
|
Socioeconomic Condition |
Low |
48 (73.8%) |
|
Middle |
12(18.5%) |
|
|
High |
5(7.7%) |
|
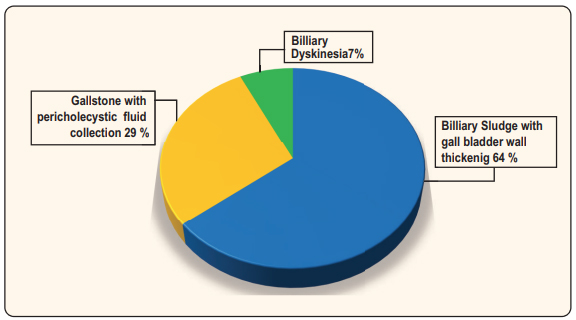
Regarding socioeconomic condition, 48(73.8%) patients were from low socioeconomic background whereas patients from the middle class and higher-class background were of 12(18.5%) and 5(7.7%) respectively. As illustrated the clinical manifestations the most common symptom was upper abdominalpain 57(87.69%) followed by fever and chills 55(84.6%), anorexia 53(81.5%), vomiting, 52(80.0%), nausea 47(72.3%), constipation, 25(38.8) & itching 13 (20.0%). Among the observed presenting sings all the patients 65(100%) had right upper quadrant &/or epigastric tenderness, 46(70.8%) had muscle guard or rigidity, 33 (50.8%) were with jaundice and 26 (40.0%) were presented with palpable mass over the right upper abdominal quadrant. From clinical presentations, duration of symptoms, laboratory, radiological and sonological findings 42 patients (64.6%) out of 65 was diagnosed as acute cholecystitis preoperatively and the rest 23 patients (53.6%) was diagnosed as chronic cholecystitis. In patients of acute cholecystitis, the preoperative findings included biliary sludge with thickening of gall bladder wall 64.0% was the major finding, then gallstone with pericholecystic fluid collection in 29.0% cases and then biliary dyskinesia in 7.0% cases (Figure 1).
|
Clinical Characteristics |
|
Results |
|
|---|---|---|---|
|
Presenting symptoms |
Upper abdominal pain |
57(87.7%) |
|
|
|
Fever and chills |
55 (84.6%) |
|
|
|
Anorexia |
53 (81.5%) |
|
|
|
Vomiting |
52 (80.0%) |
|
|
|
Nausea |
47 (72.3%) |
|
|
|
Constipation |
25 (38.5%) |
|
|
|
Itching |
13 (20.0%) |
|
|
Presenting signs |
Right upper quadrant and/ or epigastric tenderness |
65 (100.0%) |
|
|
|
Muscle guard/ rigidity |
46 (70.8%) |
|
|
|
Jaundice |
33 (50.8%) |
|
|
|
palpable tender mass over the right upper abdominal quadrant |
26 (40.0%) |
|
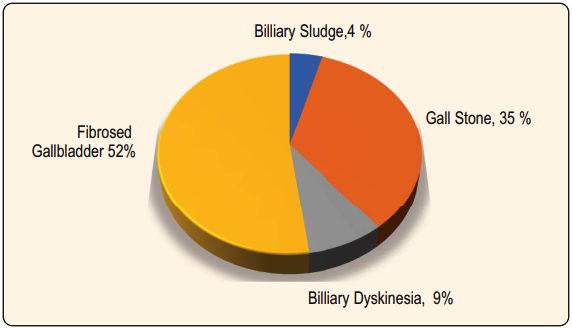
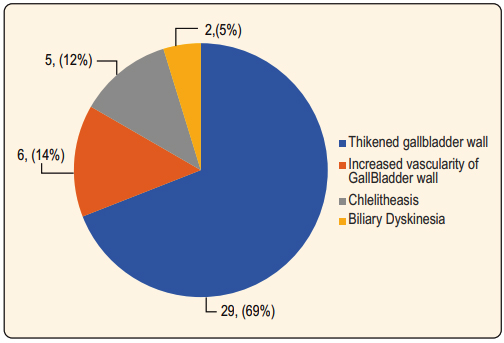
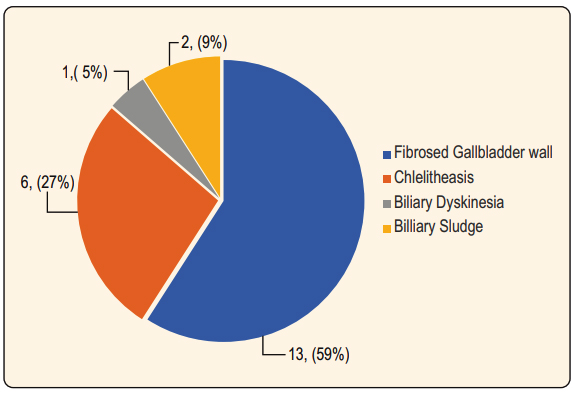
Contrary to this, in chronic cholecystitis majority of the patients (52.0%) had fibrosis of gallbladder wall and then 35.0% had gall stone, 9.0% had biliary dyskinaesia and only 4.0% had biliary sludge (Figure 2). The post-operative results were mostly based on per operative findings and histopathological report (biopsy report and noted that in acute cases (Figure 3). the thickened gallbladder wall was the major findings (69.0%), then features of raised vascularity of gall bladder wall (14.0%) then cholelithiasis (12.0%) and biliary dyskinesia (5.0%) respectively. In chronic cases fibrosis of gallbladder wall was the most common (57.0%) finding and this is followed by cholelithiasis (30.0%), biliary sludge (9.0%) and biliary dyskinesia (4.0%) (Figure 4).
On the observed results of association of several clinical diseases and pathogens with cholecystitis, out of 65 patients, total 37 (56.4%) cases had been found to have a relation with prior disease or pathogens. 25(23.9%) were associated with acute cholecystitis and rest 12(13.1%) were with chronic cholecystitis (table III).
|
Pattern of diseases and pathogens with number |
No. in acute cholecystitis |
No. in chronic cholecystitis |
||||
|---|---|---|---|---|---|---|
|
Bacterial |
26 |
Typhoid enteritis |
10(15.4%) |
6 |
4 |
|
|
|
|
Urinary tract infection |
7(10.8%) |
6 |
2 |
|
|
|
|
Acute gastroenteritis |
4(6.2%) |
4 |
- |
|
|
|
|
Hepatitis |
3(4.6%) |
2 |
1 |
|
|
|
|
Pneumonia |
2(3.1%) |
2 |
- |
|
|
Viral |
4 |
Influenza |
2(3.1%) |
2 |
- |
|
|
|
|
Herpes simplex infection |
1(1.5%) |
1 |
- |
|
|
|
|
Cytomegalovirus infection |
1(1.5%) |
1 |
- |
|
|
Others |
7 |
Thalassemia |
4(6.2%) |
|
4 |
|
|
|
|
Helminthiasis |
3(4.6%) |
1 |
2 |
|
|
Total |
37 |
|
37(56.4%) |
25(23.9%) |
12(13.1%) |
|
The most common observed infectious diseases associated with cholecystitis was typhoid
enteritis (15.4%) which was followed by urinary tract infection (10.8%), acute gastroenteritis (6.2%), hepatitis (4.6%) and pneumonia (3.1%). The common associated viral pathogens were influenza (3.1%) and then herpes simplex and cytomegalovirus (3.1% equally both). Besides infectious disease, 6.2% cases belong to thalassemia and 4.6% cases was with helminthic infestation.
|
Category |
Acute cholecystitis |
Chronic cholecystitis |
Totals |
|---|---|---|---|
|
Prior infestation with pathogens |
25 (23.9) [0.05] |
12 (13.1) [0.09] |
37 |
|
Without prior infestation with pathogens |
17 (18.1) [0.07] |
11 (9.9) [0.12] |
28 |
|
Column Totals |
42 |
23 |
65 |
Results of the association of prior infestation with pathogens and cholecystitis were analysed. The means that the result was not significant 0.567188. The previous pathogenic infestation was not independent with cholecystitis and there had a relation between cholecystitis and previous history of clinical diseases and pathogens (p=0.5671).
Discussion
Though many studies reported on raising incidence of cholecystitis and cholecystectomy in children, however, elaboration on nature of the cholecystitis is still underestimated.6,8 Recent advances in medical technology, however, has made a vivid change in diagnosis of spectrum of gallbladder diseases with their management.9
In current study though the sample size was not very large (n = 65), however, it was sufficient to be considered representative of the general population as cholecystitis is not so common in children and the study period was too short. Here, the socio- demographic results showed that, the mean age of the study population 8.35 years (Mean SD 8.35± 1.27) was co related with the two relevant studies where the mean ages ranging was from 7.8 to 9.0 years.10,11 In terms of sex ratio very little difference was observed between the two groups and that was 1.166 (male and female 35, & 30 respectively). This sex distribution was also in line with those of relevant studies.10-12 Here, most of the patients 48 (73.8%) were from low socioeconomic background whereas 12(18.5%) and 5(7.7%) patients were from middle and higher-class family respectively. These results correspond with the study of Bhasin SK et al where, among 80 patients, 67.5% (n = 54) belonged to lowsocioeconomic status and 32.5% (n = 26) from middle class.23 This represent that though previously it has been thought that cholecystitis has a strong relationship with upper class family with high calorie consumption but now the scenario may have been changed.
Regarding clinical manifestation, in both acute and chronic cholecystitis cases, the most common symptom was found upper abdominal pain 57 (87.7%) followed by chills with fever 55 (84.61%) and then anorexia (81.5%), vomiting (80.0%), nausea (72.0%), constipation (38.5%) and itching (20.0%) and the most common sign was right upper quadrant or epigastric tenderness 65(100.0%), then muscle guard or rigidity (70.8%), jaundice (50.8%) and 26(40.0%) were presented with palpable mass over the right upper abdominal quadrant. These results noted that in both cases (acute or chronic) upper abdominal colicky pain 57(87.7%.) was the commonest symptom and right upper quadrant tenderness 65(100.0%) was the commonest sign. This is because, most of the signs and symptoms were overlapped in either cases of acute and chronic cholecystitis and hence by clinical presentation a clean-cut differentiation of acute and chronic cases was very difficult. This is correlated with the several relevant studies where the clinical presentation was also regarded as quite unspecific and the diagnosis was challenging1,3,10,13.
Interestingly, in this study, there was no variation in proportion of pre and post operatively diagnosed cases of acute and chronic cholecystitis though there remain variation in findings. This result contradicts with the study result of Brain P Blackwood and Grabowski study where the frequency of chronic cholecystitis was more than acute one and there was a little variation in pre and post-operative diagnostic findings.1 This might be due to small sample size of current study. However, in several other studies this distribution has a positive correlation.10,12
On laboratory data analysis of this study, liver function tests (serum bilirubin level, alkaline phosphatase level, alanine aminotransferase (ALT) level and coagulation profile), CRP level, triple antigens, blood culture and bacterial culture report noted that patients with acute attack were with higher level of tests results than chronic attack and particularly cholecystitis associated with infective causes had much higher level of serum bilirubin, CRP and blood leucocytes count. The results corelate with the study results of Lu YA et al and Poddighe D et al where in acute cholecystitisalanine aminotransferase (ALT) level, leucocytes count, blood culture and bacterial culture test results showed more raised.10,20
The preoperative findings revealed that biliary sludge was the commonest findings (64.0%) in acute cholecystitis, then gallstone (29.0%) and biliary dyskinesia (7.0%). On the contrary, in chronic cholecystitis, majority of the patients (52.0%) had fibrosis of gallbladder wall, 35.0% had gall stone, 9.0% had biliary dyskinesia and only 4.0% was with biliary sludge. This means that in acute cases acalculouscholecystitis and biliary sludge was the major findings whereas in chronic cases fibrosis of gallbladder was the major findings and in both acute and chronic cholecystitis though gallstone was an important finding but in chronic cholecystitis its proportion was more significant. These findings corelate with those reported in the relevant literature.10,14-16
The post-operative results illustrated that thickened gallbladder wall and raised vascularity of gallbladder wall was the major findings (69.0% and 57.0% respectively) in acute cholecystitis whereas fibrosis of gallbladder walls and features of cholelithiasis (57% and 30% respectively) were the major finding in chronic cholecystitis. Besides, biliary dyskinesia which was another finding account for 5.0% in acute and 4.0% in chronic cholecystitis respectively. Biliary sludge was another considerable finding (9.0%) in chronic cholecystitis. These results symbolise that in paediatric population cholecystitis whatever acute or chronic may often presents with various findings without gallstone. The results have similarity with those reported in the relevant literatures.1,16-17
In current study, out of 65 patients 37 (56.4%) cases with cholecystitis had been found to have relation with prior disease or pathogens. The commonly observed associated infectious diseases were typhoid enteritis (15.4%) followed by urinary tract infection (10.8%) then cute gastroenteritis (6.2%), hepatitis (4.6%) and pneumonia (3.1%) respectively. The associated viral pathogens were influenza (3.1%), herpes simplex and cytomegalovirus (3.1% equally in both). Besides infectious disease, 6.2% cases belong to thalassemia and 4.6% cases with helminthic infestation had association with cholecystitis. This indicates that, the previous pathogenic infestation is not independent with cholecystitis and there had a relation between cholecystitis and previous history of clinical diseases and pathogens. This study results suggest that prior evaluation is important to identify the associated risk factors that might cause cholestasis and that results cholecystitis in children. In some relevant studies of several authors there are also found association between several diseases and pathogenic infestation with cholecystitis.3,12 Most of these authors findings were though with acute acalculouscholecystitis, however, in current study the association was also noted in both acute and chronic cases but separately it was not statistically analysed because of small sample size.
Conclusion
Acute acalculouscholecystitis with biliary sludge accounts for the majority of paediatric cholecystitis and there was an association between paediatric cholecystitis with prior infestation of disease pathogens.
As the current study was a single centred one with limited a sample size with short duration with a set criteria and parameters. So, it is to reflect the total scenario of paediatric cholecystitis among Bangladeshi children. Hence, to ascertain a complete picture with an advance outcome, a large scale nationally representative sample involving other tertiary hospitals and health centres of the country recommended.
References
- Blackwood PB, Grabowski J. Chronic cholecystitis in the pediatric population: an underappreciated disease process. GastroenterolHepatol Bed Benc 2017;10:125-130.
DOI: 10.22037/ghfbb.v0i0.980 - Bhasin SK, Gupta A, Kumari S, Evaluation and management of cholelithiasis in children: a hospital-based study, IntSurg J. 2017;4:246-251.
DOI: 10.18203/2349-2902.isj20164450 - Karami H, Kianifar HR, Karami S Cholelithiasis in Children: A Diagnostic and Therapeutic Approach, J Pediatr Rev. 2017;5: e9114.
DOI: 10.17795/jpr-9114 - Walker SK, Maki AC, Cannon RM, Foley DS, Wilson KM, Galganski LA, Wiesenauer CA, Bond SJ, Etiology and incidence of pediatric gallbladder disease, Surgery. 2013;154:927-933.
DOI: 10.1016/j.surg.2013.04.040 - Silva IV, Reis AF, Palaré MJ, Ferrão A, Rodrigues T, Morais A. Sickle cell disease in children: chronic complications and search of predictive factors for adverse outcomes. Eur J Haematol. 2015; 94: 157-61.
DOI: 10.1111/ejh.12411 - Srinath AI, Youk AO, Bielefeldt K. Biliary dyskinesia and symptomatic gallstone disease in children: two sides of the same coin? Dig Dis Sci. 2014; 59: 1307-15.
DOI: 10.1007/s10620-014-3126-2 - Mehta S, Lopez ME, Chumpitazi BP, Mazziotti MV, Brandt ML, Fishman DS. Clinical characteristics and risk factors for symptomatic pediatric gallbladder disease. Pediatrics. 2012; 129: e82-8.
DOI: 10.1542/peds.2011-0579 - Svensson J, Makin E. Gallstone disease in children. Semin Pediatr Surg. 2012;21: 255-65.
DOI: 10.1053/j.sempedsurg.2012.05.008 - Tucker JJ, Grim R, Bell T, Martin J, Ahuja V. Changing demographics in laparoscopic cholecystectomy performed in the United States: hospitalizations from 1998 to 2010. Am Surg. 2014; 80: 652-8.
DOI: 10.1177/000313481408000718 - Poddighe D, Tresoldi M, Licari A, and Marseglia GL, Acalculous Acute Cholecystitisin Previously Healthy Children: General Overview and Analysis of Pediatric Infectious Cases, International Journal of Hepatology. 2015:1-6.
DOI: 10.1155/2015/459608 - Huffman JL, and Schenker S. Acute acalculouscholecystitis: a review. Clin Gastroenterol Hepatol. 2010; 8:15–22.
DOI: 10.1016/j.cgh.2009.08.034 - Imamoðlu M, Sarihan H, Sari A, Ahmetoðlu A, Acute acalculouscholecystitis in children: Diagnosis and treatment, J Pediatr Surg. 2002;37:36-9.
DOI: 10.1053/jpsu.2002.29423 - Raptopoulos V, Carolyn C, Paul Doherty, Edward H. Smith, Carl J. D’Orsi, NilimaA. Patwardhan Robert Goldberg, Chronic Acalculous Gallbladder Disease: Multiimaging Evaluation with Clinical- Pathologic Correlation AJR Am J Roentgenol. 1986;147:721-4.
DOI: 10.2214/ajr.147.4.721 - Shreders A, Michie C, AcalculousCholecystitis in 14 years old Boy with no predisposing factor. The West London Medical Journal. 2010;2:11-14.
DOI: - Suh SG, Choi Y-S, Park K-W, and Lee SE Pediatric cholecystectomy for symptomatic gallstones unrelated to hematologic disorder, Ann Hepatobiliary Pancreat Surg. 2016;20:187–90.
DOI: 10.14701/ahbps.2016.20.4.187 - Jessica Y Ngand Jennie Gu ,Conservative Management of Acalculous Cholecystitis in a Seven-year-old Child,Cureus. 2018;10: e2092. Published online 2018 Jan 20.
DOI: 10.7759/cureus.2092 - Bailey PV, Connors RH, Tracy TF Jr, Sotelo-Avila C, Lewis JE, Weber TR. Changing spectrum of cholelithiasis and cholecystitis in infants and children. Am J Surg. 1989; 158:585-88.
DOI: 10.1016/0002-9610(89)90199-2 - Deepak J, Agarwal P, Bagdi RK, Balagopal S, Madhu R, Balamourougane P, Pediatric cholelithiasis and laparoscopic management: A review of twenty two cases,J Minim Access Surg. 2009;5:93–96.
DOI: 10.4103/0972-9941.59306 - Velev V1, Tolekova N, Naidenova N, Stoilov S, Nansenova V and Sopotenski, Acalculouscholecystitis in child in the cource of salmonella gastroenteritis, Clinical Case with a Review of the Literature Pediatric Infectious Diseases. 2018;3:3 http.//www.imedpub.com jan 19, 2018.
DOI: 10.4172/2573-0282.100059 - Lu YA, Chiu CH, Kong MS, Wang HI, Chao HC, Chen CC Risk factors for poor outcomes of children with acute acalculouscholecystitis, Pediatr Neonatol. 2017;58:497-503.Epub 2017 Mar 25.
DOI: 10.1016/j.pedneo.2016.12.005 - Barie, P. and Eachempati, S. Acute acalculous- cholecystitis. Gastroenterol Clin North Am. 2010; 39:343–357.
DOI: 10.1016/j.gtc.2010.02.012 - Kang JY, Ellis C, Majeed A, Hoare J, Tinto A, Williamson RC, et al. Gallstones—an increasing problem: a study of hospital admissions in England between 1989/1990 and 1999/2000. Aliment Pharmacol Ther. 2003; 17:561-69.
DOI: 10.1046/j.1365-2036.2003.01439.x
Department of Pediatric Surgery, Shaheed Suhrawardy Medical College Hosital, Dhaka, Bangladesh
dr.nirupamasaha@yahoo.com
 0000-0003-3486-677X
0000-0003-3486-677X
Submission
04 October 2020
Accepted
17 October 2021
Published
01 December 2021
Apply citation style format of Bangladesh Medical Research Council
Issue
Vol 47 No 3 (2021)
Section
Research Articles
Ethical Clearance
IRB of Shaheed Suhrawardy Medical College and Hospital, Dhaka, Bangladesh.
Financial Support
Bangladesh Medical Research Council, Dhaka, Bangladesh.
Conflict of Interest
Authors have no conflict of interest.