Sheikh Farhana Huda
Department of Gynaecological Oncology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh.
Fawzia Hossain
Department of Gynaecological Oncology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh.
Muhammad Jasim Uddin
Department of Gynaecological Reproductive Endocrinology and Infertility,Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh.
Kaniz Farhana
Department of Gynaecological Oncology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh.
Shah Md Mahfuzur Rahman
Institute of Public Health, Dhaka, Bangladesh.
Keywords: Epithelial ovarian cancer; CT scan; Cytoreductive surgery; CA-125
DOI: 10.3329/bmrcb.v47i3.59993
Abstract
Background: Globally, among gynaecologic cancers, ovarian cancer represents higher morbidity and mortality. Approximately, 90% of ovarian cancer are epithelial in origin. Primary cytoreductive surgery followed by chemotherapy is the cornerstone of treatment for epithelial ovarian cancer. Suboptimal cytoreduction may result in surgical complications and delay in chemotherapy which are against survival. Therefore, it is important to predict patients who are unlikely to achieve optimum cytoreduction.
Objectives: To evaluate the preoperative clinical, laboratory and radiographic parameters to predict feasibility of optimum cytoreduction in advanced stage epithelial ovarian cancer.
Methods: This prospective observational study was conducted at the department of gynaecological oncology, Bangabandhu Sheikh Mujib Medical University, Dhaka between January 2020 to December 2020. Thirty-one malignant epithelial ovarian cancer cases were enrolled through purposive sampling. Clinical history, physical examination, preoperative CA 125 and total platelet count were noted. CT scan based on FIGO staging 2014 was compared to the surgical staging. Maximum surgical effort for cytoreduction was achieved and the risk factors for sub-optimal cytoreduction were identified.
Results: Optimal cytoreduction was achieved in 64.5% cases. There was difference between optimal and suboptimal cytoreduction regarding CA125 and total platelet count (TPC) (p = <0.05). In CT scan, there was difference too, regarding liver involvement (p =0.048), peritoneum (p =0.024), hydroureter (p=0.003) and lymphadenopathy (p =0.000). Multivariate logistic regression analysis showed that peritoneal involvement (OR= 13.500, 95% CI (1.340-135.983)) in CT scan, significantly increase the risk of suboptimal cytoreduction.
Conclusion: Preoperative CA125 >500U/ml and total platelet count >450×109/L and peritoneal involvement, liver involvement, lymphadenopathy and hydroureter in preoperative CT scan are important predictor of suboptimal cytoreduction.Keywords: Epithelial ovarian cancer; CT scan; Cytoreductive surgery; CA-125.
Introduction
Ovarian cancer is one of the most common and lethal diseases among females worldwide.1 In 2020, The American Cancer Society estimated 21,750 new cases of ovarian cancer and estimated deaths 13,940 due to this fatal disease.2 According to GLOBOCAN 2020, worldwide 313959 new cases were diagnosed, and 207252 deaths were recorded in ovarian cancer and it is the 8th most common cancer both in incidence (6.6%) and mortality (4.2%) among female.3 In Bangladesh, ovarian cancer is an alarming health problem and GLOBOCAN reported 3122 new cases and 2096 deaths due to ovarian cancer in year 2020 and incidence is 3.9% and mortality 2.9%.4
Ovarian cancer are a heterogenous group of malignancies. Among them epithelial ovarian cancers are most common, and accounting 90% of all cases.5 Epithelial ovarian cancer are highest in women aged 55 to 64 years and deaths are highest in women aged 75 to 84 years.6 Currently, more than 75% of ovarian cancer diagnosed at advanced stage and their 5 years survival rate is less than 30%.7 Nonspecific symptoms and lack of reliable biomarkers are responsible for delayed diagnosis.8
Primary cytoreductive surgery followed by chemotherapy is the standard management of advanced stage epithelial ovarian cancer and extent of residual disease after surgery is an important predictor of prognosis.9 However, in some cases primary surgery is avoided because of associated uncontrolled medical disorder or unresectable tumor. If optimum cytoreduction is not possible neoadjuvant chemotherapy followed by interval debulking surgery is a good alternative.10 The prognosis of patients with ovarian cancer is directly related to the tumor stage during diagnosis and presence of residual tumor burden after cytoreductive surgery. Gynecologic oncology group (GOG) defined “optimal debulking” if residual tumor volume is <1cm.11 Currently, the primary goal of primary cytoreductive surgery has been changed to R0 resection with absence of any macroscopic disease. A meta-analysis found every 10% improvement in maximum cytoreduction resulted in an incremental improvement in overall survival of 5%.9 So the most important prognostic factor for overall survival of is maximal diameter of residual tumor after surgery.12,13 The 5 years survival rate for the patients with complete cytoreduction is 60%, whereas for optimal cytoreduction it is 35% and the 5 years survival rate is only 20% for the patients who had suboptimal cytoreduction.14 Neoadjuvant chemo- therapy has been associated with shorter operative times, fewer surgical complications and reduction in organ resections.15 A prospective randomised study (EORTC 55971) found that neoadjuvant chemotherapy followed by interval debulking surgery was not inferior to primary debulking surgery for advanced stage epithelial ovarian cancer.13
Many studies done to predict the role of CA-125, imaging and laparoscopy for prediction of optimal debulking but yielded conflicting results. 16The changes in the CA-125 level in the perioperative period, had important prognostic and predictive information. But its practical application remains theoretical because findings are not validated prospectively. 17 A meta- analysis found CT findings had poorer predictive performance. Preoperative CT predictors should be used with caution.18 But in some studies computed tomographic presence of massive ascites, liver parenchymal involvement, suprarenal lymph node involvement, involvement of porta hepatis, extensive omental involvement, intestinal and diaphragmatic involvement, hydroureter were associated with suboptimal cytoreduction.19,20 Thrombocytosis associated with extensive initial disease burden, measurable residual disease.21 Preoperative platelet count >350 G/L was associated with suboptimal cytoreduction.22 A recent study found tumoral FABP4 as a molecular marker of residual disease.23 The aim of this study was to determine different preoperative clinical, laboratory and radiographic parameters to predict feasibility of optimum cytoreduction.
Materials and Methods
This prospective, observational study was carried out at the department of gynaecological oncology, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka from January-December 2020. A total of 31 patients with clinically, biochemically and radiologically diagnosed advanced stage epithelial ovarian cancer (EOC) who underwent primary cytoreductive surgery were included in the study. Patient who had taken NACT, synchronous abdominopelvic pathology, medically unfit patient (age>80yrs, ASA class > 3), non-epithelial and metastatic ovarian cancer were excluded from the study. Fourteen participants were excluded due to nonmalignant condition and early stage disease.
Informed written consent was taken and confidentiality maintained. Data on clinical history, physical examination, laboratory investigations (CBC, CA125), imaging (abdominopelvic CT scan) and per-operative findings were collected. Pre-anaesthetic checkup and ASA class identified. Patients whose preoperative evaluation suggested an advanced stage ovarian malignancy, underwent laparotomy.
Ascites: Ascites was classified as mild, moderate and marked, according to American Society of Anaesthesiology (ASA) class:24
ASA Class I: A normal healthy patient;
ASA Class II: A patient with mild systemic disease;
ASA Class III: A patient with severe systemic disease;
ASA Class IV: A patient with severe systemic disease that is a constant threat to life;
ASA Class V: A moribund patient who is not expected to survive without the operation; and
ASA Class VI: A declared brain-dead patient whose organs are being removed for donor purposes. 25
Laboratory tests: Preoperative serum CA125 > 500 U/ ml and thrombocytosis were associated with suboptimal cytoreduction.21,22,26 In this study, level of CA- 125 500 U/ml and total platelet count 450×109//L was considered as cut off value.
Preoperative computed tomographic scan: Preoperative multiple axial non-contrast and contrast (oral and IV) CT scan was performed one month before operation. The images were reviewed by consultant radiologist. In this study, stage IIB to stage IV was considered as advanced stage disease.27
Surgical treatment: A midline abdominal incision was recommended for thorough surgical staging and maximal cytoreduction included total abdominal hysterectomy, bilateral salpingo-oophorectomy, total omentectomy, appendectomy, surgical removal of all tumor masses, intestinal resections (if required) and enlarged lymphadenectomy. Achievement of no gross residual tumor was attempted in all cases. Finally, patients were divided into 2 groups:
• Optimal cytoreduction with no residual or £1cm residual tumor
• Sub optimal group with >1cm residual tumor
Surgical risk factors for suboptimal cytoreduction were noted as:
• Hard fixed lump.
• Parenchymal liver involvement
• Omental cake
• Bowel involvement
• Peritoneal carcinomatosis- defined as disease >4 mm involving 2 or more of the following areas; para colic gutter, anterior abdominal wall, diaphragm and pelvic peritoneal reflections.
• Pelvic side wall involvement
Data analysis and interpretation: Statistical analysis was carried out by using Statistical Package for Social Science version 23.0 for Windows (SPSS inc, Chicago, Illinois, USA). Qualitative data were presented as number and percentage while quantitative data were presented as mean, standard deviations and ranges. Comparison was done by Chi-square test. The confidence interval set to 95%. The p value <0.05 was considered significant.
Results
Respondents were of 25-70 years age group. Some forty two percent respondents belonged to less than 50 years. Majority of the population (64.5%) were of postmenopausal period, and 77.4% respondents were multiparous. Out of 31 respondents 70.9% were of normal BMI and 83.8% were mildly anaemic. About 48.4% cases were in ASA class 2 (table 1). Of the study population, 17 (54.8%) population had CA 125 >500U/ml and maximum population (74.2%) had total platelet count £450×109/L (table I).
|
Characteristics |
Frequency |
Percentage |
|---|---|---|
|
Age |
||
|
<50 yrs |
12 |
41.9% |
|
50-59 yrs |
10 |
32.3% |
|
60-69 yrs |
07 |
22.6% |
|
70-79 yrs |
01 |
3.2% |
|
|
Mean ±SD: 50.84±10.80 |
Min –Max: 25-70 |
|
Menopausal status |
|
|
|
Premenopausal |
21 |
35.48% |
|
Postmenopausal |
20 |
64.52% |
|
Parity |
||
|
Multiparous |
24 |
77.40% |
|
Primiparous |
07 |
22.60% |
|
BMI |
||
|
18.5-24.9 |
22 |
70.96% |
|
25-29.9 |
08 |
25.84% |
|
³ 30 |
01 |
3.22% |
|
Anemia |
||
|
Mild |
26 |
83.87% |
|
Moderate |
05 |
16.31% |
|
ASA class |
||
|
1 |
13 |
41.94% |
|
2 |
15 |
48.39% |
|
3 |
03 |
09.68% |
|
CA 125(U/ml) |
||
|
£500 14 |
45.16 |
|
|
>50017 |
54.84 |
|
|
Total platelet count |
||
|
>450×109/L |
08 |
25.80% |
|
£450×109/L |
23 |
74.20% |
In CT scan, liver involvement was absent among the maximum (93.6%) cases. Pelvic side wall involvement, diaphragm involvement, bowel involvement was absent in all 31 cases. Other CT scan findings were ascites where most of the patients (58.1%) had moderate ascites. Maximum 77.4% were in stage III disease, 19.4% had lymph adenopathy and 9.7% had pleural effusion and 22.6 % respondents had omental and peritoneal involvement (table II).
|
Variables |
CT findings |
Surgical findings |
|---|---|---|
|
Liver |
2(6.45%) |
7(22.6%) |
|
Diaphragm |
0 |
5(16.1%) |
|
Omentum |
7(22.58%) |
23(74.2%) |
|
Peritoneum |
7(22.58) |
13(41.94%) |
|
Pelvic side wall |
0 |
3(9.7%) |
|
Bowel |
0 |
6(19.35%) |
|
Hydroureter |
4(12.9%) |
5(16.1%) |
|
Lymphadenopathy |
6(19.35%) |
10(32.26%) |
|
Ascites Mild |
7(22.58%) |
5(16.13%) |
|
Moderate |
18(58.07%) |
19(61.30%) |
|
Marked |
6(19.35%) |
7(22.60%) |
|
Pleural effusion |
3(9.68%) |
………… |
|
Stage II |
4(12.9%) |
7(22.58%) |
|
Stage III |
24(77.42%) |
20(64.52%) |
|
Stage IV |
3(9.68%) |
4(12.9%) |
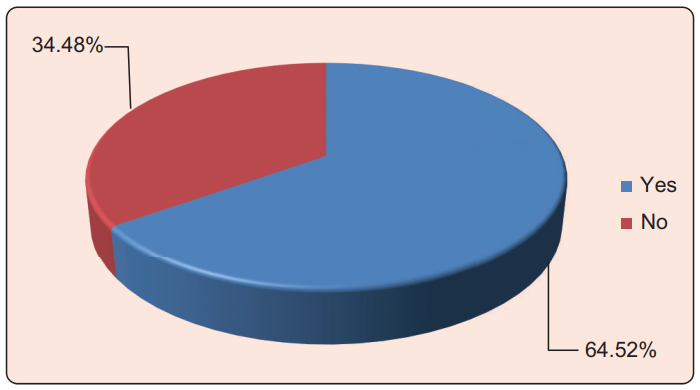
Per- operatively liver involvement, diaphragm involvement was absent among the maximum cases (77.4%) and (83.9%) respectively. Furthermore, peritoneal involvement (58.1%), pelvic side wall involvement (90.3%), bowel involvement (80.6%) and lymphadenopathy (67.7%) were absent in per operative findings (table II). Optimal cytoreduction was achieved in 64.5% cases and suboptimal cytoreduction occurred 35.5% cases (Figure 1). There was no statistically significant difference between women with optimal and suboptimal cytoreduction regarding age of the patients, menopausal status, anemia, BMI and ASA class (table III). There was significant difference in CA125 and total platelet count (TPC) where (p <0.05; table III).
|
Variables |
Optimal cytoreduction |
pvalue |
|
|---|---|---|---|
|
Yes |
No |
||
|
Age |
|
|
|
|
<50 |
10(50.0%) |
3(27.3%) |
0.556 |
|
50-59 |
5(25.0%) |
5(45.5%) |
|
|
60-69 |
4(20.0%) |
3(27.3%) |
|
|
70-79 |
1(5.0%) |
0 |
|
|
Menopausalstatus |
|
|
|
|
Premenopausal |
8(40.0%) |
3(27.3%) |
0.495 |
|
Postmenopausal |
12(60.0%) |
8(72.7%) |
|
|
Anemia |
|
|
|
|
Mild |
18(90%) |
8(72.7%) |
0.224 |
|
Moderate |
2(10%) |
3(27.3%) |
|
|
BMI(kg/m2) |
|
|
|
|
18.5-24.9 |
15(75.0%) |
7(63.63%) |
0.669 |
|
25-29.9 |
5(25.0%) |
3(27.27%) |
|
|
≥30 |
0 |
1(9.1%) |
|
|
ASAclass |
|
|
|
|
1 |
8(40.0%) |
5(45.5%) |
0.800 |
|
2 |
10(50.0%) |
5(45.5%) |
|
|
3 |
2(10%) |
1(9.1%) |
|
|
CA125(U/ml) |
|
|
|
|
≤500 |
13(65.0%) |
1(9.1%) |
0.02 |
|
>500 |
7(35.0%) |
10(90.9%) |
|
|
Total platelet count/L |
|
|
|
|
>450×109 |
2(10.0%) |
6(54.55%) |
0.000 |
|
≤450×109 |
18(90.0%) |
5(45.45%) |
|
In computed tomography, only peritoneal (p=0.024), hydroureter (p=0.003) and lymphadenopathy (p=0.000) had statistically significant difference in optimal and suboptimal cytoreduction. But there was no statistically significant difference between women with optimal and sub optimal cytoreduction regarding liver, diaphragm, omental, pleural effusion, bowel involvement, ascites and stages (table IV).
|
CT findings |
Involvement |
Optimal cytoreduction |
pvalue |
|
|---|---|---|---|---|
|
Yes |
No |
|||
|
Liver |
Present |
0.0 |
2(18.2%) |
0.051 |
|
|
Absent |
20(100%) |
9(81.8%) |
|
|
Diaphragm |
Absent |
20(100%) |
11(100%) |
NV |
|
Omental |
Present |
4(20.0%) |
3(27.3%) |
0.656 |
|
|
Absent |
16(80.0%) |
8(72.7%) |
|
|
Peritoneal |
Present |
2(10.0%) |
5(45.5%) |
0.024 |
|
|
Absent |
18(90.0%) |
6(54.5%) |
|
|
Pelvic Side Wall |
Absent |
20(100%) |
11(100%) |
NV |
|
Hydroureter |
Present |
0.0 |
4(36.4%) |
0.003 |
|
|
Absent |
20(100%) |
7(63.6%) |
|
|
Pleural Effusion |
Absent |
2(10.0%) |
1(9.1%) |
0.937 |
|
|
Present |
18(90.0%) |
10(90.9%) |
|
|
Bowel Involvement |
Absent |
20(100%) |
11(100%) |
NV |
|
Lymphadenopathy |
Present |
0.0 |
6(54.5%) |
0.000 |
|
|
Absent |
20(100%) |
5(45.5%) |
|
|
Ascites |
Absent |
0.0 |
0.0 |
0.843 |
|
|
Mild |
5(25.0%) |
2(18.2%) |
|
|
|
Moderate |
11(55.0%) |
7(63.6%) |
|
|
|
Marked |
4(20.0%) |
2(18.2%) |
|
|
Stage |
Stage II |
4(20.0%) |
0.0 |
0.787 |
|
|
Stage III |
13(65.0%) |
11(100%) |
|
|
|
Stage IV |
3(15.0%) |
0.0 |
|
There was significant difference between women with optimal and suboptimal cytoreduction regarding liver involvement (p=0.001), diaphragm involvement (p=0.023), peritoneal involvement (p=0.000), omental involvement (p=0.014), hydroureter (p=0.000) in per-operative findings.
Correlation between CT findings and surgical findings showed peritoneal involvement, liver involvement, lymphadenopathy had 100.0% specificity and 100.0% positive predictive value (p=0.006, 0.048 and 0.005 respectively; table V).
|
T findings |
SurgicalFindings |
p value |
Sensitivity |
Specificity |
PPV |
NPV |
||
|---|---|---|---|---|---|---|---|---|
|
Yes (7) |
No (24) |
|||||||
|
Liver* |
Yes |
2(28.57%) |
0 (0.0%) |
0.048* |
28.57% |
100% |
100% |
82.75% |
|
|
No |
5 (71.43%) |
24 (100%) |
|
|
|
|
|
|
|
Yes (13) |
No (18) |
|
|
|
|
|
|
|
Peritoneal* |
Yes |
7 (53.85%) |
0 (0.0%) |
0.006 |
53.85% |
100% |
100% |
75% |
|
|
No |
6 (46.15%) |
18 (100%) |
|
|
|
|
|
|
|
Yes (5) |
No (26) |
|
|
|
|
|
|
|
Hydroureter* |
Yes |
3 (60%) |
1 (3.85%) |
0.007 |
60% |
96.15% |
75% |
92.59% |
|
|
No |
2 (40%) |
25 (96.15%) |
|
|
|
|
|
|
|
Yes (10) |
No (21) |
|
|
|
|
|
|
|
Lymphadenopathy* |
Yes |
6 (60%) |
0 (0.0%) |
0.005 |
60% |
100% |
100% |
84% |
|
|
No |
4 (40%) |
21 (100%) |
|
|
|
|
|
Data are presented number (percent)
Pearson Chi square test
*Statistically significant
Multivariate logistic regression analysis for the predictors of optimal cytoreduction showed that the only predictors of optimal cytoreduction was CT peritoneal involvement (p <0.05). The multivariate logistic regression results showed that peritoneal involvement (OR= 13.500, 95% CI (1.340-135.983)) in computed tomography, significantly increase the risk of suboptimal cytoreduction (table VI).
|
CT Findings of: |
B |
S.E. |
Sig. |
OR |
95% C.I. for OR |
|
|---|---|---|---|---|---|---|
|
Lower |
Upper |
|||||
|
Liver involvement |
1.404 |
44670.570 |
1.000 |
4.073 |
.000 |
. |
|
Peritoneal involvement |
2.603 |
1.179 |
.027 |
13.500 |
1.340 |
135.983 |
|
Hydroureter |
1.198 |
44670.570 |
1.000 |
3.315 |
.000 |
. |
|
Lymphadenopathy |
21.517 |
44119.224 |
1.000 |
2211476020.788 |
.000 |
. |
|
Constant |
-2.197 |
.745 |
.003 |
.111 |
|
|
Discussion
In this study, optimal cytoreduction was found in 64.5% cases in accordance with Abd-Elhameed et al where optimum cytoreduction was achieved in 62% cases.20 Arab et al found 71.3% of patients underwent optimal cytoreduction where both early and advanced stages were included. The mean age was 50.84±10.81 years, and range was 25-75 years. Arab et al in their study found the mean age was 50.92±12.65 years.28 Suidan et al found age ³60 years was significantly associated (p=0.001) with suboptimal debulking.19
Mean age and age difference may be due to ethnic, genetic, geographic variation and racial influence of study population. Of the study population, 64.5% patients were of postmenopausal period (p=0.495), no difference was to be found between optimal and suboptimal cytoreduction in accordance with Abd-Elhameed et al and Nithya et al (p = 0.089 and 0.12 respectively.20,29 83.87% had mild anaemia in accordance with Arab et al (p= 0.735) 28. Furthermore, 70.9% had normal BMI (p=0.669) in accordance with Son et al (p =0.84.30
In this study, 54.8% patients had CA 125 > 500 U/ml and 45.2% had £500 U/ml. CA 125 was statistically significant (p=0.02) which are consistent with the findings of Janco et al and Suidan et al (p<0.001).19,31
In our study, total platelet count (p=0.000) was significant in accordance with Janco et al and Arab et al where preoperative total platelet count was >450×109/L and predictive value was 0.009 and 0.014 respectively for suboptimal cytoreduction.28,31
Computed tomographic presence of peritoneal involvement had (p=0.006), specificity 100.0%, PPV 100.0%, which are similar with Son et al, and statistically significant on univariate and multivariate analysis (p= 0.010 and 0.025 respectively).30
Janco et al and Naik et al found statistical significance of peritoneal involvement (p=0.006 and p=0.001 respectively); but opposite findings was found in the study of Nithya et al (p=0.209, specificity 56.5%, PPV 54.5%).29,31,32 This difference might be due to inclusion of both primary and interval cytoreductive cases.
In CT scan, presence of hydroureter was had p value 0.007 and specificity 96.15%, PPV 75%, was similar to the study done by Abd-Elhameed et al where p value was 0.018.20 CT findings of lymphadenopathy was related to suboptimal cytoreduction (p= 0.005, specificity 100.0%, PPV 100.0%) which is consistent with Nithya et al.29
CT findings of liver involvement was significant in this study (p= 0.048, specificity 100.0% and PPV 100.0%) which is in aggreement with the Arab et al and Abd- Elhameed et al studies (p= 0.041 and < 0.001 respectively).20,28
There was no statistically significant difference between optimal and suboptimal cytoreduction regarding involvement of diaphragm, omentum, pelvic side wall, bowel, presence of ascites, pleural effusion and preoperative staging.
Hu et al found large volume ascites had the highest sensitivity (64.0%) for suboptimal cytoreduction. This discordance provably due to more study population had moderate ascites in present study.
Abd-Elhameed et al found significant difference between optimal and suboptimal cytoreduction regarding pelvic side wall encasement (p=0.006), pleural effusion (p=0.001) and preoperative staging (p=0.001) detected at CT scan discordance with present study probably due to small sample size.20
A multivariate logistic regression was performed of computed tomographic liver involvement, peritoneal involvement, hydroureter, lymphadenopathy and shown peritoneal involvement [OR=13.500, CI=95% (1.340-135.983)] significantly increased the risk of suboptimal cytoreduction.
Multivariate logistic regression analysis done by Abd- Elhameed et al for the predictors of optimum cytoreduction and shown, the only predictors of optimum cytoreduction were CT stage and hydroureter.20
Conclusion
Based on the findings of this study, it may be concluded that preoperative CA-125 and total platelet count, preoperative computed tomographic findings of peritoneal involvement, hydroureter and lymphadenopathy were significantly associated with suboptimal cytoreduction. Per operative findings of liver involvement, diaphragm involvement, peritoneal involvement, pelvic side wall involvement and presence of hydroureter also had significant effect on suboptimal cytoreduction. Limitation of this study included purposive sampling and it was conducted at a very short period of time. Due to the Covid 19 pandemic situation, there was small sample size and the data collection was challenging.
Acknowledgments
The authors gratefully acknowledge the support of women with ovarian malignancy who consented to be a part of this study and all hospital staff of Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh.
References
- Feng Z, Wen H, Jiang Z, Liu S, Ju X, Chen X, et al. A triage strategy in advanced ovarian cancer management based on multiple predictive models for RO resection: a prospective cohort study. Journal of Gynaecological Oncology. 2018;25:1-11.
- Siegel RL, Miller KD, Jemal A. Cancer Statistics. A Cancer Journal for Clinicians.2020;70:7-30.
- GLOBOCAN 2020 Ovarian cancer in World. accessed December 16 2020.
- GLOBOCAN 2020 Ovarian cancer in Bangladesh. accessed December16 2020.
- Wentzensen N, Poole EM, Trabert B, White E, Arslan AA, Patel, AV. Ovarian cancer risk factors by histologic subtypes: An analysis from the ovarian cancer cohort consortium. Journal of Clinical Oncology.2016;34:2888-98.
- Surveillance, Epidemiology and End Results (SEER) Program. Bethesda MD: National Cancer Institute, National Institutes of Health. USA. 2016.
- Siegel RL, Miller KD, Jemal A. Cancer Statistics. A Cancer Journal for Clinicians.2017;6:7-30.
- Devan SM, Pailoor J, Sthaneshwar P, Narayan V. Pattern of tissue expression of CA-125 and HE4 in primary epithelial ovarian tumors and correlation with serum CA-125 levels. Asian Pacific Journal of Cancer Prevention. 2013; 14:4545-8.
- Bristow RE, Tomacruz RS, Armstrong DK, Trimble EL, Montz FJ. Survival effect of maximal cytoreductive surgery for advanced ovarian carcinoma during the platinum era: a metaanalysis. Journal of Clinical Oncology. 2002; 20:1248-59.
- Tangjitgamol S, Hanprasertpong J, Cubelli M, Zamagni C. Neoadjuvant chemotherapy and cytoreductive surgery in epithelial ovarian cancer. World Journal of Obstetrics and Gynecology. 2013;2:153-66.
- Hoskins WJ, McGuire WP, Brady MF, Homesley HD, Creasman WT, Berman M, et al. The effect od diameter of largest residual disease on survival after primary cytoreductive surgery in patients with suboptimal residual epithelial ovarian carcinoma. American Journal of Obstetrics and Gnecology. 1994;170:974-9.
- Mousavi AS, Mazhari MM, Mitra M, Guilani MM, Behtash N, Akhavan S. Can primary optimal cytoreduction be predicted in advanced epithelial ovarian cancer preoperatively?.World Journal of Surgical Oncology.2013;.8:11.
- Vergote I, Trope CG, Amant F, Kristensen GB, Ehlen T, Johnson N et al. European organization for research and treatment of cancer-gynaecological cancer group; NCIC Clinical trials group. Neoadjuvant chemotherapy or primary surgery in stage IIIC or IV ovarian cancer. New England Journal of Medicine.2010;363:943-53.
- Bristow RE. (2007) Primary cytoreductive surgery for advanced stage ovarian cancer: Indications for radical resections. Cancerologia 2. 2007; Suppll:s31-s36.
- Meyer LA, Cronin AM, Sun CC. Use and effectiveness of neoadjuvant chemotherapy for treatment of ovarian cancer. Journal of Clinical Oncology.2016;34:3854-63.
- Ibeanu OA, Bristow RE. Predicting the outcome of cytoreductive surgery for advanced ovarian cancer:a review. International Journal of Gynecological Cancer. 2010;20:S1-11.
- Diaz-Pallida I, Razak AR, Minig L, Bernardini MQ, Maria DC.Prognostic and predictive value of CA-125 in the primary treatment of epithelial ovarian cancer:potentials and pitfalls. Clinical and Translation Oncology. 2012;14:15-20.
- Hu TWY, Nie D, Gou JH, Li ZY. Predictive significance of preoperative CT findings for suboptimal cytoreduction in advanced ovarian cancer: a meta-analysis. Cancer Management and Research. 2018; 10:2019-30.
- Suidan RS, Ramirez PT, Sarasohn DM. A multicenter assessment of the ability of preoperative computed tomography scan and CA-125 to predict gross residual disease at primary debulking for advanced epithelial ovarian cancer. Gynecologic Oncology.2014;145:27-31.
- Abd-Elhameed NA, Elshamy ME, Elhameed TA. The preoperative predictors of optimal cytoreductive surgery in women with advanced epithelial ovarian cancer. International Invention Journals.2016;3:205-11.
- Allensworth SK, Langstraat CL, Martin JR, Lemens MA, Mcgree ME, Weaver AL, et al. Evaluating the prognostic significance of preoperative thrombocytosis in epithelial ovarian cancer. Journal of Gynaecological Oncology 2013;130:499-504.
- Slabuszewska-Jozwiak A, Dmoch-Gajzlerska E, Kozakiewicz B, Jakiel G. The prognostic significance of thrombocytosis in ovarian cancer. Annals of Agricultural and Environmental Medicine.2015;22:731-35.
- Tucker SL, Herbrich SM, Unruh AK, Nick AM, Crane EK, Coleman RL, et al. Molecular biomarkers of residual disease after surgical debulking of high-grade serous ovarian cancer. Clinical Cancer Research. 2014;20:3280-8.
- KASHANI A, LANDAVERDE C, MEDICI V, ROSSARO L. Fluid retention in cirrhosis: pathophysiology and management. An International Journal of Medicine.2008;101:71-85.
- Adapted from National institute for Health and Care Excellence. NICE guideline 45: routine preoperative tests for elective surgery, 2016. Available at https:// www.nice.org.uk/guidance/ng45. Accessed July 7, 2019.
- Chi DS, Venkatraman ES, Masson V, Hoskins WJ. The Ability of Preoperative Serum CA125 to Predict Optimal Primary Tumor Cytoreduction in Stage III Epithelial Ovarian Carcinoma. Journal of Gynaecological Oncology. 2000;77:227-31.
- FIGO Committee on Gynecologic oncology: Prat, J. (2014) Staging classification for cancer of the ovary, fallopian tube, and peritoneum. International Journal Gynaecology and Obstetrics.124:1-5.
- Arab M, Jamdar F, Hosseini MS. Ghodssi-Ghasemabadi R, Farzaneh F, Ashrafganijoei T.Model of prediction of optimal debulking of epithelial ovarian cancer. Asian Pacific Journal of Cancer Prevention 2017;19:1319-24.
- Nithya S, Jayalakshmi D, Barathi D, Dubashi B. Preoperative prediction of surgical outcome in advanced ovarian cancer by computed tomographic scan and Eastern Cooperative Oncology Group-performance status. International Journal of Reproduction, Contraception, Obstetrics and Gynecology. 2018;7:3672-77.
- Son HM, Kim SH, Kwon BR, Kim MJ, Kim CS, Cho SH. Preoperative prediction of suboptimal resection in advanced ovarian cancer based on clinical and CT parameters. The Foundation Acta Radiologica.2016;0:1-7.
- Janco JMT, Glaser G, Kim B, McGree ME, Weaver AL, Cliby WA, et al. Development of a prediction model for residual disease in newly diagnosed advanced ovarian cancer. Elsevier.2015;138:70-77.
- Naik R, Suchitra R, Naik B. Comparative study of pre- operative CT scan and per-operative findings in carcinoma ovary. International Journal of Reproduction, Contraception, Obstetrics and Gynecology.2015;4:1367-73.
Department of Gynaecological Oncology, Bangabandhu Sheikh Mujib Medical University, Shahbagh, Dhaka, Bangladesh.
md487@yahoo.com
 0000-0001-5192-2863
0000-0001-5192-2863
Submission
16 August 2021
Accepted
17 October 2021
Published
01 December 2021
Apply citation style format of Bangladesh Medical Research Council
Issue
Vol 47 No 3 (2021)
Section
Research Articles
Ethical Clearance
Institutional Review Board (IRB) of Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh.
Financial Support
Bangladesh Society for Colposcopy and Cervical Pathology (BDSCCP), Dhaka, Bangladesh.
Conflict of Interest
There was no conflict of interest.