Md. Mahfuzar Rahman
Department of Community Medicine, Anwer Khan Modern Medical College, Dhanmondi, Dhaka, Bangladesh.
Md Atiqur Rahman
Department of Community Medicine, Anwer Khan Modern Medical College, Dhanmondi, Dhaka, Bangladesh.
Abu Kawser Sarker
Department of Community Medicine, Anwer Khan Modern Medical College, Dhanmondi, Dhaka, Bangladesh.
Md Abu Rayhan Miah
Health Services Division, Ministry of Health and Family Welfare, Dhaka, Bangladesh.
Keywords: Non-communicable diseases, Risk factors, Sustainable Development Goals, School health programme
DOI: 10.3329/bmrcb.v47i3.59240
Abstract
Background: Globally, two third of world’s deaths are due to non communicable diseases (NCDs). Preventable risk factors of NCDs are associated with life style modification and behaviour pattern which are largely dependent on the practices adopted in younger age.
Objective: This was an exploratory type of cross-sectional study using mixed method (Quantitative and Qualitative) approach.
Methods: The study was conducted in randomly selected four schools in two divisions of the country in two randomly se lected Upazilas. Data were generated using pretested structured questionnaire & by Focus Group Discussion (FGDs). This was an exploratory type of cross-sectional study using mixed method (Quantitative and Qualitative) approach.
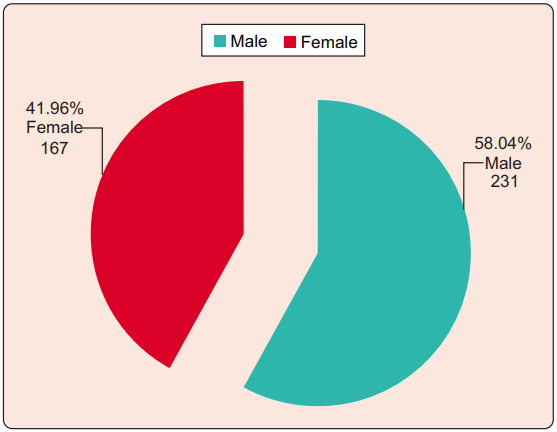
Results: In this study about 54.0% respondents were found above 15 years of age with a mean of 14.1 years ±1.66. Among the respondents 58.04% were male and 41.96% were female. The study revealed that the respondents had family history of diabetes, hypertension, and use of tobacco among 40.2%, 44.5%, and 34.7% respectively. The respondents (79.9%) generally were aware about NCDs, however (20.1%) were unaware too. The various aspects of the level of knowledge on NCDs, risk factors and their information sources were agreed upon among by 60-85% respondents. More than 70.0% respondents were aware and agreed upon about the complications of NCDs as heart disease, stroke, blindness, paralysis, kidney disease and liver diseases in particular. In response to attitude towards prevention 65-80% respondents had the positive attitudes towards the different aspect of NCDs prevention. However, it was negative in regard to daily dietary inclusion of vegetables; homeopathic and ayurbedic medicine for NCDs treatment options to about 40-70% respondents respectively.
Conclusion: This study finding highlights the needs for developing strategies in building and implementing awareness among school children at large under existing school health programme of the country towards NCDs prevention and control.Keywords: Non-communicable diseases, Risk factors, Sustainable Development Goals, School health programme
Introduction
Non-communicable diseases (NCDs) have emerged as serious public health problem worldwide. Generally it affects all the populations around the globe but mostly among low- and middle income populations in particular. As a consequences of economic transition there is a shift in the diseases spectrum from communicable diseases to non-communicable diseases (NCDs).1 Cardiovascular diseases, diabetes mellitus, and stroke have emerged as major NCDs of public health importance in India, with high morbidity and mortality affecting the most economically productive years of life making a challenge to society and the economy of the nation.2 Currently, more than 35 million people die from NCDs each year worldwide representing nearly two third of world’s deaths. Most of these deaths (>80%) are in low and middle income countries and occur before the age of 60.3 NCDs have some common risk factors such as tobacco use, unhealthy diet, physical inactivity, high alcohol consumption, raised blood pressure (BP), and excess body adiposity. The development of policies and programmes focusing on reducing the burden of these common risk factors are likely to make a substantial impact on mitigating the mortality and morbidity due to NCDs.4 The major and potentially preventable risk factors of NCDs are associated with lifestyle modification and behavior pattern which are largely depend on the practices adopted in younger age. Intermediate school children (adolescents) are known for experimentation and are vulnerable to adopt certain lifestyles which may predispose them to NCDs. The awareness and knowledge of adolescents about NCDs and their risk factors are an important part of population based prevention strategy. Assessing and appropriately disseminating knowledge of the modifiable risk factors at an early age are an essential preventive educational approach. The awareness levels in this age group could be used as a baseline on which health promotional strategies can be developed. The current cross sectional study is designed considering this context. The proportional mortality rate due to Non-Communicable Diseases (NCDs) has been increasing day by day in Bangladesh.5-9 As a result, NCDs have been identified as one of the important public health problems in the country. Major NCDs include heart diseases, stroke, diabetes, chronic respiratory diseases and cancers.9,10 They are caused by the top of genetic predisposition and age, some behavioural risk factors like unhealthy diet, tobacco use, physical inactivity, and excessive use of alcohol over a prolonged period.11 It gradually mature to metabolic risk factors such as hypertension, impaired glucose tolerance, dyslipidaemia, and ultimately develop into full blown NCDs.12
Materials and Methods
This was an exploratory type of cross-sectional study using mixed method (Quantitative and Qualitative) approach. The study was conducted in the randomly selected four schools in two divisions (Dhaka and Sylhet) of the country in two randomly selected districts Dhaka and Moulavibazar (Dhamrai and Sreemongal Upazilas) having a total of four schools from class VIII-X. Secondary school children (class VIII-X) those willing to participate were considered as study population. The study period was for six months. Simple random sampling technique was used by lottery method in selecting divisions, districts, upazilas and schools respectively. Data were collected from 398 respondents through face to face interview using a pre-tested structured questionnaire with prior filling up a consent form and signed by the respondents. Four Focus Group Discussions (FGDs) were took place in four schools (One in each school) according to moderator’s guide that consisted of 12-15 school children as respondents. After collecting data, it was checked for consistency, and cleaned, compiled, edited and analysed manually and by using appropriate computer programme. The statistical tests were done to analyse descriptive statistics with the mean, standard deviation. Data were presented in the form of tables and diagrams as appropriate. Interpretation of study findings were made by descriptive statistical tests.
Results
There were equal number (50.0%) of respondents in schools of each division. About 54.0% respondents were found above 15 years of age. Mean age: 14.1 ± 1.66 years (table-I).
|
Age in years |
No. of respondents |
Percentage |
|---|---|---|
|
12-13 |
95 |
23.9 |
|
14-15 |
88 |
22.1 |
|
>15 |
215 |
54.0 |
|
Total |
398 |
100.0 |
Mean age: 14.1 years. SD: + 1.66
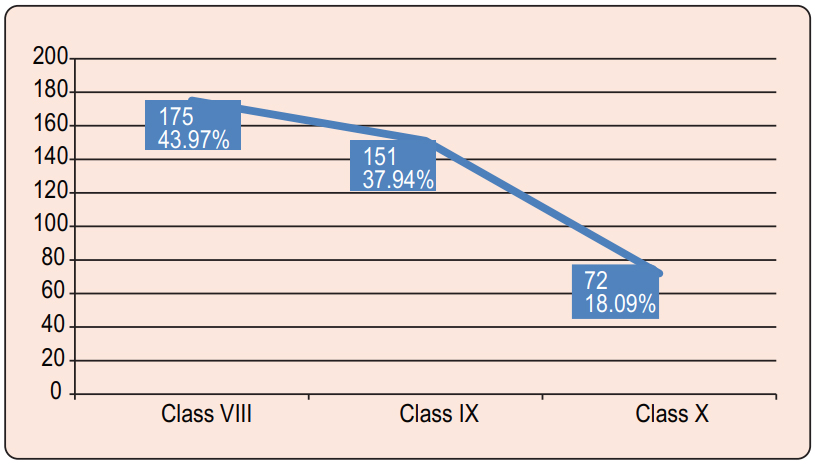
Among the respondents 58.0% were male and 41.9% were female (Figure 1) In this study most of the respondents were Muslim. The study respondents were belongs to class VIII (43.9%), class IX (37.9%) and class X (18.1%) respectively (Figure 2) Most of the respondents had the family history of diabetes, hypertension, and use of tobacco among 40.2%, 44.5%, and 34.7% respectively (table II).
|
Family history of NCDs |
No. of respondents |
Percentage |
|---|---|---|
|
Diabetes |
160 |
40.2 |
|
Hypertension |
177 |
44.5 |
|
Obesity |
64 |
16.1 |
|
Tobacco use |
138 |
34.7 |
|
Cancer |
12 |
03.0 |
|
Coronary Heart ) |
53 |
13.30 |
|
Disease (CHD |
|
|
|
Stroke |
36 |
09.0 |
The various aspects of the level of knowledge on NCDs, risk factors and their information sources were agreed upon among by 60-85% respondents. However, the information sources on NCDs risk factors from friends were agreed to about 30% respondents only (table III).
|
Statements |
SA |
A |
UD |
D |
SD |
|---|---|---|---|---|---|
|
NCDs are the diseases of risk factors rather specific causes |
48 |
228 |
68 |
27 |
27 |
|
|
(12.06) |
(57.28) |
(17.08) |
(6.79) |
(6.79) |
|
Hypertension belongs to NCDs |
94 |
188 |
62 |
26 |
28 |
|
|
(23.62) |
(47.23) |
(15.58) |
(6.54) |
(7.03) |
|
Diabetes mellitus belongs to NCDs |
99 |
195 |
56 |
32 |
16 |
|
|
(24.88) |
(48.99) |
(14.07) |
(8.04) |
(4.02) |
|
Obesity belongs to NCDs |
91 |
192 |
69 |
27 |
19 |
|
|
(22.86) |
(48.24) |
(17.33) |
(6.79) |
(4.78) |
|
Cancer belongs to NCDs |
83 |
171 |
63 |
47 |
34 |
|
|
(20.85) |
(42.98) |
(15.82) |
(11.80) |
(8.55) |
|
Coronary heart disease belongs to NCDs |
82 |
172 |
63 |
54 |
27 |
|
|
(20.60) |
(43.21) |
(15.83) |
(13.57) |
(6.79) |
|
Stroke belongs to NCDs |
53 |
227 |
55 |
36 |
27 |
|
|
(13.31) |
(57.03) |
(13.82) |
(9.05) |
(6.79) |
|
NCDs are becoming a major public health problem |
85 |
210 |
55 |
32 |
16 |
|
|
(21.35) |
(52.77) |
(13.82) |
(8.04) |
(4.02) |
|
Cigarette/berry is a risk factor for NCDs |
250 |
92 |
32 |
20 |
04 |
|
|
(62.82) |
(23.11) |
(08.04) |
(5.02) |
(1.01) |
|
Alcohol is a risk factor for NCDs |
206 |
90 |
63 |
27 |
12 |
|
|
(51.76) |
(22.61) |
(15.83) |
(6.79) |
(3.01) |
|
Obesity is a risk factor for NCDs |
204 |
105 |
64 |
20 |
05 |
|
|
(51.25) |
(26.38) |
(16.08) |
(5.03) |
(1.26) |
|
Junk food is a risk factor for NCDs |
55 |
225 |
64 |
27 |
27 |
|
|
(13.81) |
(56.53) |
(16.08) |
(6.79) |
(6.79) |
|
Anxiety is a risk factor for NCDs |
52 |
220 |
57 |
45 |
24 |
|
|
(13.06) |
(55.28) |
(14.32) |
(11.31) |
(6.03) |
|
Excess salt consumption is a risk factor for NCDs |
36 |
208 |
63 |
69 |
22 |
|
|
(9.05) |
(52.26) |
(15.83) |
(17.33) |
(5.53) |
|
Lack of physical activities is a risk factor for NCDs |
82 |
172 |
63 |
54 |
27 |
|
|
(20.60) |
(43.21) |
(15.83) |
(13.57) |
(6.79) |
|
Information on NCDs, risk factors from electronic media |
84 |
172 |
63 |
52 |
27 |
|
|
(21.11) |
(43.21) |
(15.83) |
(13.06) |
(6.79) |
|
Information on NCDs, risk factors from print media |
213 |
32 |
63 |
68 |
22 |
|
|
(53.52) |
(8.04) |
(15.83) |
(17.08) |
(5.57) |
|
Information on NCDs, risk factors from my friends |
34 |
83 |
206 |
63 |
12 |
|
|
(8.85) |
(20.85) |
(51.76) |
(15.83) |
(3.01) |
|
Information on NCDs, risk factors from teachers |
239 |
95 |
33 |
25 |
06 |
|
|
(60.05) |
(23.87) |
(8.29) |
(6.28) |
(1.51) |
|
Information on NCDs, risk factors from doctors |
93 |
192 |
68 |
27 |
18 |
|
|
(23.37) |
(48.24) |
(17.08) |
(6.79) |
(4.52) |
|
Information on NCDs, risk factors from parents |
86 |
171 |
63 |
52 |
26 |
|
|
(21.60) |
(42.98) |
(15.83) |
(13.06) |
(6.53) |
|
Information on NCDs, risk factors from other sources |
85 |
210 |
55 |
32 |
16 |
|
|
(21.35) |
(52.77) |
(13.82) |
(8.04) |
(4.02) |
The various aspects of the level of knowledge on NCDs, risk factors and their information sources were agreed upon among by 60-85% respondents. However, the information sources on NCDs risk factors from friends were agreed to about 30% respondents only.
In response to attitude towards prevention 65-80% respondents had the positive attitudes towards the different aspect of NCDs prevention. However, it was negative in regard to daily dietary inclusion of vegetables, homeopathic, and ayurbedic medicine for NCDs treatment options to about 40-70% respondents respectively (table IV).
|
Attitude towards prevention of NCDs |
Yes |
No |
|---|---|---|
|
Green leafy vegetables should be added in daily diet |
246 |
152 |
|
|
(61.81) |
(38.19) |
|
Daily seasonal fruit intake can prevent NCDs |
264 |
134 |
|
|
(66.33) |
(33.67) |
|
Avoiding excess salt intake prevent NCDs |
253 |
145 |
|
|
(63.57) |
(36.43) |
|
Daily physical activity helps preventing NCDs |
295 |
103 |
|
|
(74.12) |
(25.88) |
|
Regular medication is important for preventing NCDs |
325 |
73 |
|
|
(81.66) |
(18.34) |
|
Life style change/modification can prevent occurrence of NCDs |
264 |
134 |
|
|
(66.33) |
(33.67) |
|
Allopathic medicine is better option for the treatment of NCDs |
261 |
137 |
|
|
(65.58) |
(34.42) |
|
Homeopathic medicine is better option for the treatment of NCDs |
238 |
160 |
|
|
(59.80) |
(40.20) |
|
Ayurbedic medicine is better option for the treatment of NCDs |
122 |
276 |
|
|
(30.65) |
(69.35) |
65-80% respondents had the positive attitudes towards the different aspect of NCDs prevention. However, it was negative in regards to daily dietary inclusion of vegetables, homeopathic, and ayurbedic medicine for NCDs treatment options to about 40-70% respondents respectively.
As outcome of FGDs, it was found that about two third respondents indicates NCDs were the diseases of risk factors rather specific cause and had the knowledge of NCDs as a growing public health issues. More than two third respondents considered smoking as a major risk factor for NCDs and not good for health as well and nearly 80.0% respondents considered junk food as a risk factor for NCDs as well. On the other hand, two third respondents agreed upon about anxiety and stress as a major risk factor for NCDs too. On matter of daily physical activities more than two third respondents agreed upon its benefits in preventing NCDs. However, these issues were disagreed by one fourth of the respondents and regarding available information sources on NCDs risk factors, respondents mostly were agreed upon as electronic & print media, friend, teacher and doctors in particular. Heart, kidney diseases including stroke and paralysis were opined by two third of the respondents as the complications of NCDs and more than half of the respondents were in favor of taking green leafy vegetables and seasonal fruits. Moreover, regular physical activities and avoiding excess salt in diet were the favourable options among majority of the respondents and almost two third of the respondents were in favour of Allopathic medicine as better option for the treatment of NCDs.
Discussion
It was an exploratory type of cross-sectional study with mixed approach (Qualitative and Quantitative) among secondary school children from class VIII-X to assess the respondents’ socio-demographic characteristics, level of knowledge on NCDs risk factors, awareness on complications as well as attitude towards its preventive measures in addition to the knowledge on source of information about NCDs. It was revealed that about 54.0% respondents were above 15 years of age where mean age was 14.1 ± 1.66 years. The respondents 58.0% were male and 41.9% were female where mostly Muslim. The respondent’s family members had the history of diabetes, hypertension, and use of tobacco mostly. As our people do not use community clinics and union level health facilities for their treatment of hypertension and diabetes although these were close to their home.
The health care institutions at union and ward level need to build capacity accordingly in addressing NCDs needs of the community. The respondents about one fifth were unaware about NCDs. Several WHO report indicates the major behavioral risk factors for NCDs are modifiable, metabolic factors are preventable and the NCDs are treatable to a large extent.13,14 In this study, the knowledge on NCDs, risk factors and their information sources were agreed upon by 60-85% respondents and majority were aware and agreed upon about the complications of NCDs as heart disease, stroke, blindness, paralysis, kidney disease and liver diseases in particular. Primary Health Care (PHC) system in Bangladesh can play an important role in prevention of diseases through public awareness, early detection, treatment and referral.17 The positive attitudes towards prevention on different aspects were among 65-80% respondents however, it was negative towards daily dietary inclusion of vegetables, homeopathic, and ayurbedic medicine for NCDs treatment options to about 40-70% respondents respectively. In regard to public awareness school health programme should have the opportunity engaging children and adolescents in healthy eating, regular physical activity which can lower their risk of developing NCDs. Schools play a critical role through establishing a supportive environment for such healthy behaviors.20
Conclusion
Findings of this study suggest that there is a scope for improving awareness and knowledge of this group of children about NCDs and their risk factors as part of population based prevention strategies. The findings will also help policy makers towards development of awareness programmes necessary for implementation among school children at large to prevent NCDs related morbidity and mortality in contributing Sustainable Development Goals (SDGs) in improving quality of life from childhood.
As the present study revealed one fifth respondents were out of awareness on various issues of NCDs, therefore an immediate comprehensive NCDs awareness and health promotional programme would have been considered and developed on priority for the secondary school children through existing school health service of the country.
Acknowledgments
The authors do acknowledge gratefully the funding of the Bangladesh Medical Research Council (BMRC) in conducting this study. Our sincere thanks to the study population for their active participation as well as support staff involved in this study.
References
- Mohan V, Deepa M, Farooq S, Prabhakaran D, Reddy KS. Surveillance for risk factors of cardiovascular disease among an industrial population in Southern India.Natl Med J India 2008;21: 8 13.
- Reddy KS. Prevention and Control of Non communicable Diseases: Status and Strategies. Working paper no. 104.New Delhi: Indian Council for Research on International Economic Relations; 2003. P.30.
DOI:10419/189624 - Alwan A. Global Status Report on Non communicable Diseases 2010.Geneva, Switzerland: World Health Organization; 2011.
Available From: www.who.int/nmh/publications/ncd_report_full_en.pdf - Epping Jordan JE, Galea G, Tukuitonga C, Beaglehole R. Preventing chronic diseases: Taking stepwise action. Lancet 2005;366:1667 71.
DOI:10.1016/S0140-6736(05)67342-4 - Razzaque A, Carmichael G, Streatfield PK. Adult mortality in Matlab, Bangladesh: levels, trends, socio-demographic differentials and causes of death. Asian Popul Stud. 2009; 5: 85-100.
DOI:10.1177/1010539510392743 - Karar ZA, Alam N, Streatfield PK. Epidemiological transition in rural Bangladesh, 1986-2006.Global Health Action. 2009; 9: 2.
DOI:10.3402/gha.v2i0.1904 - Government of Bangladesh, Ministry of Health and Family Welfare. Management Information System, Dhaka.Health Bulletin. 2013.
- Zaman MM. Trends in non-communicable diseases (paper presented to the National Public Health Conference, 2013).
- World Health Organization. Non-communicable Diseases Country Profile 2014.WHO, Geneva, 2014.
- World Health Organization. Surveillance and prevention of NCD. WHO Bangladesh.
- World Health Organization. World Health Report 2002: Reducing risks, promoting healthy life. WHO, Geneva, 2002.
- World Health Organization. Global status report on non- communicable diseases 2010.WHO, Geneva, 2011.
- World Health Organization. Preventing chronic disease: a vital investment. WHO global report 2005.
- World Health Organization. Global action plan for the prevention and control of non-communicable diseases 2013- 2020.WHO, Geneva 2013.
- Anwar Islam, Tuhin Biswas. Health system in Bangladesh: challenges and opportunities. American Journal of Health Research. 2014; 2: 366-374.
DOI:10.11648/j.ajhr.20140206.18 - World Health Organization, Asia Pacific Observatory on Public Health Chronic Dis Int 3(1): id1021 (2016) - Page - 09 Zaman MM System and Policies. Bangladesh health system review. Health systems in transition. 2015; 5.
- Government of Bangladesh, Ministry of Health and Family Welfare. Health Bulletin. 2015. DGHS, Dhaka.
- Islam A, Biswas T. Chronic non-communicable diseases and the healthcare system in Bangladesh: current status and way forward. Chronic Dis Int. 2014;1: 6.
- World Health Organization. Package of essential non- communicable (PEN) disease interventions for primary health care in low-resource settings. WHO, Geneva 2011.
- O’Byrne D, Jones J, Sen Hai Y, Macdonald H. WHO, Global school health initiative. World Health. 1996;49: 5-6.
Department of Community Medicine, Anwer Khan Modern Medical College, Dhaka, Bangladesh.
mahfuzarrahman26@yahoo.com
 0000-0002-6282-7164
0000-0002-6282-7164
Submission
08 March 2021
Accepted
24 October 2021
Published
01 December 2021
Apply citation style format of Bangladesh Medical Research Council
Issue
Vol 47 No 3 (2021)
Section
Research Articles
Ethical Clearance
NREC of Bangladesh Medical Reseach Council (BMRC), Dhaka, Bangladesh.
Financial Support
Bangladesh Medical Research Council (BMRC), Dhaka, Bangladesh.
Conflict of Interest
The authors had no conflict of interest.