Mohammad Nizamul Hossain Sowdagar
Department of Cardiology, Combined Military Hospital (CMH), Dhaka, Bangladesh.
A F M Shamsul Haque
Department of Cardiology, Combined Military Hospital (CMH), Dhaka, Bangladesh.
AKM Monwarul Islam
Department of Cardiology, National Institute of Cardiovascular Diseases, Dhaka, Bangladesh.
Zahida Jabbar
Department of Ophthalmology, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh.
Syeda Aleya Sultana
Department of Cardiology, Combined Military Hospital (CMH), Dhaka, Bangladesh.
Mohammad Kamar Uzzaman Sabery Khan
Department of Cardiology, Combined Military Hospital (CMH), Dhaka, Bangladesh.
Keywords: Acute coronary syndrome, HbA1c, Atherosclerosis, Obesity.
DOI: 10.3329/bmrcb.v47i3.59235
Abstract
Background: Diabetes where glycated Hemoglobin A1c (HbA1c) level is raised, a strong independent risk factor for the development of atherosclerosis which leads to acute coronary syndrome (ACS). This study is designed to compare the in-hospital outcomes in terms of developing arrhythmias, heart failure, cardiogenic shock, cardiac arrest and death among the normal HbA1c level (<6.5%) and raised HbA1c level (≥6.5%) patients who presented with ACS.
Objective: To compare the in-hospital outcomes of patients with raised HbA1c level (≥6.5%)and normal HbA1c level (<6.5%) after first attack of acute coronary syndrome.
Methods: A total of 104 patients admitted during the study period to coronary care unit (CCU) of Combined Military Hospital (CMH), Dhaka through emergency department or chest pain unit, who suffered from acute coronary syndrome were included in this study. Patients were divided into two groups, those having HbA1c ≥6.5% and <6.5%. Patients were followed up till discharge to observe their outcome in the hospital.
Results: A total of 104 patients were included in the study where 85(81.7%) were male and 19(18.3%) were female. Gender distribution were matched in both HbA1c level (p>0.05). Risk factors including hypertension, smoking and dyslipidaemia were found significantly high among those who had HbA1c ≥6.5 (p<0.05). There was no relation with family history of CAD with higher HbA1c level. Obesity was distributed evenly in both higher and lower HbA1c levels of the diagnosis of ACS 8(7.7%) were UA, 33(31.7%) were NSTEMI and 63(60.6%) were STEMI. There were less complications among the patients who had HbA1c <6.5% (p<0.05). Arrhythmias were found to be more common in HbA1c ≥6.5% group than HbA1c <6.5% group was (p<0.05), heart failure was more in HbA1c ≥6.5% group, 10(19.2%) and (p<0.05), cardiogenic shock was found more commonly in HbA1c ≥6.5% group, 6(11.5%) (p<0.05), cardiac arrest was more 10(19.2%) among HbA1c ≥6.5% group. Finally, death was more in HbA1c ≥6.5% group. 10(19.2%) than the HbA1c <6.5% group and it was statistically significant (p<0.05).
Conclusion: Findings of the study suggest that higher HbA1c (≥6.5%) level is associated with more adverse in-hospital outcome among ACS patients.
Keywords: Acute coronary syndrome, HbA1c, Atherosclerosis, Obesity.
Introduction
Diabetes mellitus is a disease of antiquity known to mankind since the past 3500 years. Now a day’s acute coronary syndrome is a major cause of morbidity and mortality all over the world. In the Framingham study, the incidence of cardiovascular diseases in diabetic men was twofold that in nondiabetic men and in diabetic women it was threefold that in nondiabetic women.1 Hyperglycemia accelerates the process of atherosclerosis by the formation of glycated proteins and advanced glycation end products, which act by increasing the endothelial dysfunction. High admission blood glucose levels after acute myocardial infarction are common and are associated with an increased risk of death in subjects with and without diabetes. Glycometabolic state at hospital admission is an important risk marker for long-term mortality in patients with acute myocardial Infarction. Glycosylated haemoglobin provides a measure of average blood glucose levels during the period of 8 to 12 weeks. So, it could prove useful for the diagnosis of diabetes mellitus in ACS when stress induced hyperglycemia is a confounding factor as it is unlikely to rise with acute hyperglycaemia.2 With the increase of obesity, insulin resistance, and the metabolic syndrome, the worldwide prevalence of diabetes is expected to double by the year 2030. According to epidemiological characteristics, percentage of morbidity, early disability and mortality ischaemic heart disease represents a very serious socio-medical problem in the majority of countries. Epidemiological studies confirm that there is an increase in the prevalence of acute myocardial infarction (AMI) in general.3-4 Myocardial infarction is associated with a number of complications that involve the cardiac conduction system (various degrees of atrioventricular and intraventricular block); the propensity for ventricular and supraventricular arrhythmias; a variety of haemodynamic disturbances that result from contractile and diastolic ventricular dysfunction; and the mechanical disruption of intracardiac structures that leads to papillary muscle rupture with mitral regurgitation, septal rupture with left-to-right shunt, and cardiac free wall rupture with cardiac tamponade or pseudoaneurysm formation. In addition, thromboembolic events, pericarditis and recurrent ischemia or reinfarction also constitute important complications of acute myocardial infarction.5-6 In addition to being a risk factor for the development of coronary artery disease, diabetes influences outcomes following acute coronary syndrome.7-8 Considering these, the study was aimed to compare the in-hospital outcomes of patients with raised HbA1c level (≥6.5%) and normal HbA1c level (<6.5%) after first attack of acute coronary syndrome.
Materials and Methods
It was a cross sectional study done in the department of cardiology, Combined Military Hospital (CMH), Dhaka during October 2018 to June 2019. All patients presenting with first attack of acute coronary syndrome in emergency and casualty department, chest pain unit and coronary care unit of Combined Military Hospital (CMH), Dhaka during the study period. Convenient (purposive) sampling was applied to select the samples. One hundred and four subjects, 52 patients with raised HbA1c level (≥6.5%) and 52 with normal HbA1c level (<6.5%) presenting with first attack of acute coronary syndrome were purposively selected irrespective of age and sex. Each patient or his/her attendant willingly gave informed consent to take part in the study. Physically and psychologically stable patients were included in the study. Previous history of acute coronary syndrome, previous heart failure, valvular heart disease (rheumatic, congenital or degenerative), congenital heart disease, pre excitation syndrome, pregnancy, chronic kidney disease, haemoglo-binopathy, severe anaemia (Hb% <7 gm/ dl) and patient / attendant refused to give informed consent to take part in the study were excluded. All collected questionnaires were checked very carefully to identify error in the data. Data were collected from 104 patients by using predesigned questionnaires made for recording all relevant parameters under study. Statistical analysis was performed using standard statistical software (SPSS version 20). Continuous data were presented as mean ± standard deviation, categorical data were presented as frequencies and percentages. Differences between groups were evaluated using the unpaired Student t test. Chi square test was used for categorical variables and unpaired t-test was used for continuous variables. A p value of <0.05 accepted as statistically significant. Permission was obtained from the ethical committee of the hospital authority. The aims and objectives of the study along with its procedure, methods, risks and benefits of the study were explained to the patients in easily understandable language, then informed written consent were taken from the patients or legal guardians. It was assured that all information and records would be kept confident and the procedure would be helpful for both the physicians and the patients in making rational approach of the case management. They had the freedom to withdraw from the study at any time.
Results
A total of 104 patients were included in the study where 85(81.7%) were male and 19(18.3%) were female. Gender distribution were matched in both HbA1c level (p >0.05) (table I).
|
Sex |
HbA1c |
level |
Total |
|---|---|---|---|
|
<6.5% |
≥6.5% |
||
|
Male |
43(82.7%) |
42(80.8%) |
85(81.7%) |
|
Female |
9(17.3%) |
10(19.2%) |
19(18.3%) |
|
Total |
52 |
52 |
104 |
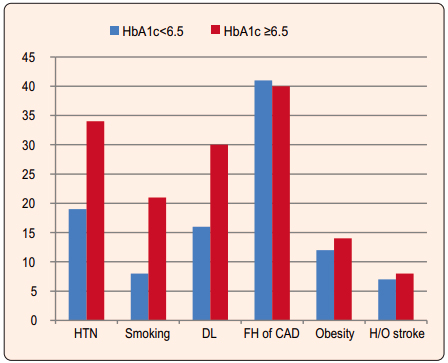
Among all 39(37.5%) were from rural origin and rest 65(62.5%) were from urban locality. Regarding risk factor analysis, in HbA1c <6.5% group hypertensive were 19(36.5%) and in HbA1c ≥6.5% group hypertensive were 34(65.4%). Distribution was significant (p<0.05). Smoking was found more in subjects who had HbA1c ≥6.5% which were 21(40.4%) and it was significant (p<0.05). Dyslipidaemia was found significantly high among those who had HbA1c 6.5% [30(57.7%)] (p<0.05). There was no relation with family history of CAD with higher HbA1c level and obesity was distributed evenly in both higher and lower HbA1c levels. There was no relation of previous history of vascular events/stroke with HbA1c level (Figure 1).
Regarding different diagnosis of ACS 8(7.7%) were UA, 33(31.7%) were NSTEMI and 63(60.6%) were STEMI (table II).
|
Diagnosis |
HbA1c |
level |
Total |
|---|---|---|---|
|
<6.5% |
≥6.5% |
||
|
UA |
4(7.7%) |
4(7.7%) |
8(7.7%) |
|
NSTEMI |
13(25.0%) |
20(38.5%) |
33(31.7%) |
|
STEMI |
35(67.3%) |
28(53.8%) |
63(60.6%) |
|
Total |
52 |
52 |
104 |
ECG changes revealed 63(60.6%) had ST elevation, 28(26.9%) had ST depression and 1(1%) had no change and 96(92.3%) had troponin I positive (table III).
|
ECG findings |
HbA1c level |
Total |
|
|---|---|---|---|
|
<6.5% |
≥6.5% |
||
|
ST elevation |
37(71.2%) |
28(53.8%) |
63(60.6%) |
|
ST depression |
12(23.1%) |
16(30.8%) |
28(26.9%) |
|
No change |
0(0%) |
1(1.9%) |
1(1.0%) |
|
Others (Dynamic changes) |
3(5.8%) |
7(13.5%) |
12(9.6%) |
|
Total |
52 |
52 |
104 |
Among all 36(34.6%) patients received SK, 57(54.8%) patients received LMWH, P.PCI was done in 7(6.7%) and others (SK followed by PCI) were done in 4(3.8%) cases (table IV).
|
Troponin I |
HbA1c level |
Total |
|
|---|---|---|---|
|
<6.5% |
≤6.5% |
||
|
Positive |
48(92.3%) |
48(92.3%) |
96(92.3%) |
|
Negative |
4(7.7%) |
4(7.7%) |
8(7.7%) |
|
Total |
52 |
52 |
104 |
Among all 36(34.6%) were given Streptokinase, 57(54.8%) were given LMWH, Primary PCI was done in 7(6.7%) and others (SK followed by PCI) were done in 4(3.8%) cases (table V).
|
Treatment |
HbA1c level |
Total |
|
|---|---|---|---|
|
<6.5% |
≥6.5% |
||
|
Streptokinase |
22(42.3%) |
14(26.9%) |
36(34.6%) |
|
LMWH |
25(48.1%) |
32(61.5%) |
57(54.8%) |
|
Primary PCI |
4(7.7%) |
3(5.8%) |
7(6.7%) |
|
Others |
1(1.9%) |
3(5.8%) |
4(3.8%) |
|
(SK+ PCI) |
|
|
|
|
Total |
52 |
52 |
104 |
There were less complications among the patients who had HbA1c <6.5% (p<0.05) (table VI).
|
Complications |
*HbA1c level |
Total |
|
|---|---|---|---|
|
<6.5% |
≥6.5% |
||
|
No |
41(78.8%) |
30(57.7%) |
71(68.3%) |
|
Yes |
11(21.2%) |
22(42.3%) |
33(31.7%) |
|
Total |
52 |
52 |
104 |
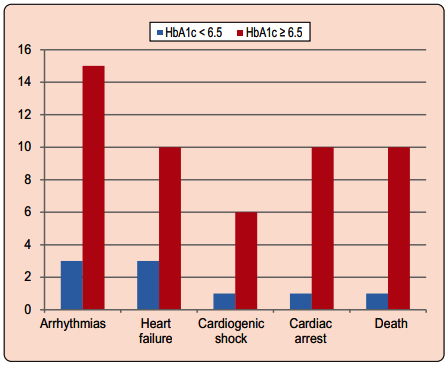
Arrhythmias were found more commonly in HbA1c ≥6.5% group than HbA1c <6.5% group which 15(28.8%) (p<0.05), heart failure was more in HbA1c ≥6.5% group than the HbA1c <6.5% group which were 10(19.2%) and p<0.05, cardiogenic shock was found more commonly in HbA1c ≥6.5% group than the HbA1c <6.5% group which were 6(11.5%) and it was significant (p<0.05), cardiac arrest was found more 10(19.2%) among HbA1c e”6.5% group than the HbA1c <6.5% group. Finally death was more HbA1c ≥6.5% group than the HbA1c <6.5% group which were10(19.2%) and it was statistically significant (p<0.05) (Figure 2).
Discussion
Acute hyperglycaemia in patients with acute coronary syndrome has several clinical implications. These patients could have established diabetes, undiagnosed diabetes or impaired glucose tolerance or stress- related hyperglycemia. Patients with diabetes or a new diagnosis of diabetes could have either established or subclinical vascular disease. The important question is whether or not hyperglycemia has independent pathophysiological effects in the clinical course of patients with acute coronary syndrome. Other studies have reported association with hyperglycaemia and mortality in acute coronary syndrome.9 In the present study, a total of 104 patients were included in the study where 85 (81.7%) were male and 19 (18.3%) were female. Gender distribution were matched in both HbA1c level (p>0.05). Among all 39(37.5%) were from rural areas and rest 65(62.5%) were from urban. These findings are taken from the sample which were purposively taken. So, it may not represent the actual scenario of Bangladesh. Regarding risk factor analysis, in HbA1c <6.5% group hypertensive were 19(36.5%) and in HbA1c ≥6.5% group hypertensive were 34(65.4%). Distribution was significant (p<0.05). Smoking was found more in subjects who had HbA1c level ≥6.5% which were 21(40.4%) and it was significant (p<0.05). Dyslipidaemia was found significantly high among those who had HbA1c level ≥6.5% [30(57.7%)] (p<0.05). There was no relation with family history of CAD with higher HbA1c level and obesity was distributed evenly in both higher and lower HbA1c levels. There was no relation of previous history of vascular events/stroke with HbA1c level. Ischemic heart disease (IHD) or coronary heart disease (CHD)] is the leading cause of death in Bangladesh and worldwide.10 Behavioral risk factors, including tobacco use, physical inactivity, and unhealthy diet are responsible for about 80% of IHD and cerebrovascular disease.11 Worldwide, hypertension is estimated to cause 7.5 million deaths, about 12.8% of the total of all annual deaths12 which is a major risk factor for IHD and strokes (Ischemic as well as hemorrhagic).13 Blood pressure levels have been shown to be positively and progressively related to the risk for stroke and coronary heart disease. In some age groups, the risk of CVD doubles for each incremental increase of 20/10 mmHg of blood pressure, starting as low as 115/75 mmHg.14 Regarding different diagnosis of ACS 8(7.7%) were UA, 33(31.7%) were NSTEMI and 63(60.6%) were STEMI. Every year in the United States, ~1.3 million patients are admitted to hospitals with UA/NSTEMI as compared with ~300,000 patients with acute STEMI. The relative incidence of UA/NSTEMI compared to STEMI appears to be increasing.15 But in our study, sample STEMI are more than that of UA/NSTEMI. ECG changes revealed 63(60.6%) had ST elevation, 28(26.9%) had ST depression and 1(1%) had no change and 96(92.3%) had troponin I positive. Among all 36(34.6%) patients received streptokinase, 57(54.8%) were given LMWH, primary PCI was done in 7(6.7%) and others (SK followed by PCI) were done in 4(3.8%) cases. There were more complications among the patients who had HbA1c level ≥6.5% <0.05). Arrhythmias were found more commonly in HbA1c ≥6.5% group than HbA1c <6.5% group (p<0.05), heart failure was more in HbA1c ≥6.5% group than the HbA1c <6.5% group which was 10(19.2%) and p<0.05, cardiogenic shock was found more commonly in HbA1c ≥6.5% group than the HbA1c <6.5% group and it was significant (p<0.05), cardiac arrest was found more 10(19.2%) among HbA1c ≥6.5% group than the HbA1c <6.5% group. In acute myocardial infarction, an increased plasma glucose level has been demonstrated to be capable of inducing such electrophysiological alterations as to favour the occurrence of arrhythmias, whose outcome could be fatal. Acute hyperglycemia is independently associated with impaired left ventricular function and with a larger infarct size due to an increased incidence of the no-reflow phenomenon. Finally, a worse myocardial performance has been demonstrated in patients with acute myocardial infarction and concomitant hyperglycemia.15 The value of HbA1c measurements for the interpretation of hyperglycemia after ACS and the estimation of the prevalence of unrecognized diabetes among patients admitted to coronary care unit with the use of fasting plasma glucose (FPG) level of 140 mg/dl and HbA1c level of more than 6.5% as combined diagnostic criteria, the study concluded that HbA1c determination is useful for early and accurate interpretation of hyperglycemia following ACS.16 A study done by Saleem et al found seventy- eight patients (70.9%) had DM, 73 (93.58%) had HbA1c >7%, 52 (47.3%) were hypertensive, 19 (17.3%) had a history of smoking and 37 (33.6%) had raised cholesterol. Coronary angiography was carried out in 87 (79.1%) patients and the severity of disease was assessed using the Gensini score. The mean Gensini score was 53.36±36.94 and the mean HbA1C was 8.4±2.39%. There was a significant association between Gensini score and DM (p=0.003) and between Gensini score and hypertension (p=0.018). HbA1C (r=0.427, p=0.001) and duration of DM (r=0.362, p=0.004) had a positive linear correlation with the Gensini score. Multiple regression analysis showed HbA1C to be an independent factor that influenced the Gensini score (p=0.021).20Our study findings also found to be associated with adverse outcome who had higher HbA1c level. Finally death was more in HbA1c ≥6.5% group than the HbA1c <6.5% group and it was statistically significant (p<0.05) High admission blood sugar levels after acute myocardial infarction are associated with increased risk of death.17 Glycometabolic state at hospital admission is an important risk marker for long-term mortality in patients with acute myocardial infarction.18 Hyperglycaemia following acute myocardial infarction may results from stress or may be due to previously unrecognized diabetes mellitus.19 Itis also found in another study that high HbA1c is associated with bad outcome instable angina patients.21 Our study also revealed that the adverse outcomes are more in those who had higher HbA1c level. It is frequently difficult to separate the two conditions clinically. Hence, blood sugar estimation alone cannot be taken as an independent diagnostic tool for hyperglycaemia with ACS, rather HbA1c may be an additional important diagnostic tool.
Conclusion
In hospital outcome of acute coronary syndrome patients vary according to the level of baseline HbA1c. Raised HbA1c level e.g., ≥6.5% are associated with adverse in-hospital outcome in ACS patients when compared to normal HbA1c level e.g. <6.5%. Complications like significant arrhythmias, heart failure, cardiogenic shock, cardiac arrest and death were more commonly observed in ACS patients with raised HbA1c level in comparison to the counterparts with normal HbA1c level.
Acknowledgments
Authors are grateful to Prof. Maj Gen Abdul Ali Mia (Retd), Prof. Maj Gen Md Azizul Islam, my guide, other departmental colleagues and staffs. Our special respect to patients who took part in this study.
References
- Kannel W, McGee D. Diabetes and cardiovascular risk factors: the Framingham Study. Circulation 1979; 59:8-13.
DOI:10.1001/jama.241.19.2035 - Y. Ramesh Naidu, Y. Sharmila, Y.Nischal, V. Srinivas, V. Satyaprasad. “Study of HbA1c levels in Acute Coronary Syndrome”. Journal of Evolution of Medical and Dental Sciences. 2015; 4:13274-78.
DOI:10.14260/jemds/2015/1909 - Bernard J. Gersh, Barry J. Maron, Robert O. Bonow, Joseph A. Dearani, Michael A. Fifer, Mark S. Link, Srihari S. Naidu, Rick A. Nishimura, Steve R. Ommen, Harry Rakowski, Christine E. Seidman, Jeffrey A. Towbin, James E. Udelson, and Clyde W. Yancy. Circulation. 2011; 124:e783-e831.
DOI:10.1016/j.jacc.2011.06.011. - Lipscombe LL, Hux JE. Trends in diabetes prevalence, incidence, and mortality in Ontario, Canada 1995-2005: a population-based study. Lancet. 2007; 369:750-56.
DOI:10.1016/S0140-6736(07)60361-4. - ESC guidelines for management of acute myocardial infarction in patient’spresenting with ST segment elevation. European Heart Journal. 2017; 4:1-66.
DOI:10.1093/eurheartj/ehx393 - Non –ST- Elevation Acute Coronary Syndromes: Executive summary, Journal of American College of Cardiology. 2014; 10:1016- 121.
DOI:10.1161/CIR.0000000000000133 - Danaei G, Lawes CM, Vander Hoorn S, Murray CJ, Ezzati M. Global and regional mortality from ischaemic heart disease and stroke attributable to higher-than-optimum blood glucose concentration: comparative risk assessment. Lancet. 2006; 368:1651-59.
DOI:10.1016/S0140-6736(06)69700-6 - Yusuf S, Reddy S, Ounpuu S, Anand S. Global burden of cardiovascular diseases, part II: variations in cardiovascular disease by specific ethnic groups and geographic regions and prevention strategies. Circulation. 2001; 104:2855-64.
DOI:10.1161/hc4701.099488 - Kosiborod M, Deedwania P. An overview of glycemic control in the coronary care unit with recommendations for clinical management. J Diabetes Sci Technol. 2009; 3:1342–51.
DOI:10.1177/193229680900300614 - Alwan A, Maclean DR, Riley LM, d’Espaignet ET, Mathers CD, Stevens GA, et al. Monitoring and surveillance of chronic non-communicable diseases: progress and capacity in high-burden countries. Lancet. 2010, 376:1861-68.
DOI:10.1016/S0140-6736(10)61853-3 - WHO. Global health risks: mortality and burden of disease attributable to selected major risks. Geneva: World Health Organization, 2009.
Available from:wiki.cancer.org.au/policy/Citation:World_Health_ Organization_2009_3 - Policy and action for cancer prevention. Food, nutrition, and physical activity: a global perspective. Washington, DC, World cancer research fund/American Institute for Cancer Research. 2009.
Available from:www.wcrf.org/dietandcancer - Whitworth JA. World Health Organization/ International Society of Hypertension statement on management of hypertension. J Hypertens. 2003;21:1983-92.
DOI:10.1097/00004872-200311000-00002 - Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, Jones DW, Materson BJ, Oparil S, Wright JT Jr, Roccella EJ; National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee. The eleventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003; 289,2560-72.
DOI:10.1001/jama.289.19.2560 - Ceriello A. Acute hyperglycemia: A new risk factor during myocardial infarction. European Heart J. 2005; 26:328.
DOI:10.1093/eurheartj/ehi049 - Soler NG, Frank S. Value of glycosylated haemoglobin measurements after acute myocardial infarction. JAMA. 1981;246:1690-93.
PMID:7277644 - Timmer JR, Vander Horst ICC, Ottervanger JP, Henriques JPS, Hoorntje JCA, Boer MJ et al. Prognostic value of admission glucose in non-diabetic patients with myocardial infarction. Am Heart J. 2004; 148:399-403.
DOI:10.1016/j.ahj.2004.04.007 - Norhammar A, Tenerz A, Nilsson G, Hamsten A, Efendic S, Ryden L et al. Glucose metabolism in patient with acute myocardial infarction and no previous diagnosis of diabetes mellitus : A prospective study. Lancet. 2002; 359:2140-44.
DOI:10.1016/S0140-6736(02)09089-X - Husband DJ, Alberti KGMM, and JulianDG.Stress hyperglycemia during acute myocardial infarction: An indicator of pre-existing diabetes. Lancet. 1983:179-81.
DOI:10.1016/s0140-6736(83)90169-1 - Saleem T, Mohammad KH, Abdel-Fattah MM, Abbasi AH. Association Of Glycosylated Haemoglobin Level and diabetes mellitus duration with the severity of coronary artery disease Diabetes Vasc Dis Res. 2008; 5:184–89.
DOI:10.3132/dvdr.2008.030 - Hong LF, Lin L, Gau UL, Luo SH, Zhu CG et al. Glycosylated hemoglobin A1c as a marker predicting the severity of coronary artery disease and early outcome in patients with stable angina Lipids Health Dis. 2014; 13: 89
DOI:
Combined Military Hospital (CMH) Dhaka, Dhaka Cantonment, Dhaka, Bangladesh.
daiyan53@yahoo.com
 0000-0003-0428-6723
0000-0003-0428-6723
Submission
13 August 2020
Accepted
28 October 2021
Published
01 December 2021
Apply citation style format of Bangladesh Medical Research Council
Issue
Vol 47 No 3 (2021)
Section
Research Articles
Ethical Clearance
Ethical committee of Armed Forces Medical Services, Dhaka.
Financial Support
Self-funded
Conflict of Interest
There is no conflict of interest.