Anisa Jahan
Child Development & Neurology Unit, Dhaka Shishu Hospital, Dhaka, Bangladesh.
Dilara Begum
Child Development & Neurology Unit, Dhaka Shishu Hospital, Dhaka, Bangladesh.
Keywords: Infantile spasm, Seizure outcome, Prednisolone, Vigabatrin
DOI: 10.3329/bmrcb.v47i3.59236
Abstract
Background: Infantile Spasm (IS) is a unique age specific epileptic encephalopathy of infancy leading to uncontrolled seizures and mental retardation. Corticosteroid and adrenocorticotropin have long been used in the treatment of infantile spasm. Vigabatrin (VGB), a suicidal inhibitor of GABA transaminase, was found to be very effective in the control of spasms. Other drugs have uncertain efficacy in controlling seizure.
Objective: To assess the seizure outcome in children with infantile spasm after treatment.
Methods: This observational study was done in a specialised paediatric neurology clinic of the Anwar Khan Modern Hospital, Dhaka. Documents of children with diagnosis of infantile spasm who was brought from November 2002 to August 2009 were reviewed. Children suspected as neuro-metabolic or neuro-degenerative disease were excluded. Also, if the children did not turn up at all or came for follow up only once within 3 months after receiving treatment were excluded from the study.
Results: A total of 110 children were enrolled in this study. Sixty nine percent children developed spasm within 3 months to 1 year of age. Mean age at first and at last examination was 10.9 months and 2.1years respectively. In 80 (72.7%) cases, seizure was ‘completely controlled’ and in 9 (8.2%) it was ‘much controlled’. But in 21(19.1%) cases the seizure was ‘not controlled’ or ‘poorly controlled’. Oral prednisolone controlled seizure in 46(41.8%) cases. ACTH was tried in 17(15.5%) children. Of these, in five (4.5%) cases seizure was completely cured. Out of 32(29.1%) babies where vigabatrin was tried , 21(19.1%) cases responded to vigabatrin . Seizure was controlled in 10 (9.1%) cases with combination of other drugs.
Conclusion: Oral prednisolone, a cheaper drug, can effectively be used as a first choice for the control of infantile spasm. Vigabatrin is good but very costly.
Keywords: Infantile spasm, Seizure outcome, Prednisolone, Vigabatrin.
Introduction
Infantile Spasm (IS) is a unique age specific epileptic encephalopathy of infancy leading to uncontrolled seizures and mental retardation.1 Infantile spasm is divided into three categories- idiopathic, symptomatic or cryptogenic. This distinction is important because a poor prognosis is to be expected in patients with structural brain damage.2 The frequent onset of infantile spasms in infancy suggests that an immature central nervous system may be important in the pathogenesis. The brain-adrenal axis also may be involved.2 The clinical response to adrenocorticotropic hormone (ACTH) and glucocorticoids can be explained by suppression of corticotropin-releasing hormone (CRH) production.2 Corticosteroid (predominantly prednisolone and hydrocortisone) and Adreno- corticotropin have long been used in the treatment of infantile spasm for over long 50 years.3 They are considered as mainstay in the treatment of IS.4-5
It is generally accepted that oral corticosteroids or ACTH will reduce or stop IS and normalize EEG findings in between 50% and 75% of patients within a week or two of starting treatment.6-9 Other antiepileptic drugs namely, sodium valporate, benzodiazepines, phenobarbitone have uncertain efficacy in the management of IS.10 Vigabatrin (VGB), a suicidal inhibitor of GABA transaminase, was first introduced in IS with tuberous sclerosis (TS) and found to be very effective in the control of spasms.11,12 The primary objective of this study was to observe the outcome of seizure after treatment in children with infantile spasm. The secondary objective was to understand which drug can be used for treatment in Bangladesh. No such study was done in Bangladesh till now.
Materials and Methods
A total of 110 children were enrolled in this observational study, done in a private specialised paediatric neurology clinic in Anwar Khan Modern Hospital, Dhaka. This clinic has been established in the year 2000, in a private hospital set up. A paediatric neuro- physician, a developmental therapist and a counselor include in this setting. Children with neurological and neuro-developmental problems are only consulted here. Thorough history, examination findings, investigations and management at first visit and in the subsequent follow up visits are well preserved for each children.
Children with clinical diagnosis of infantile spasm were included in the study. Series of myoclonic flexion or extension of the body or limbs in early childhood, which is the very characteristic of such seizure, was clinically diagnosed as infantile spasm.
Child with history of suspected neuro-metabolic or neuro-degenerative disease was excluded from the study. If the children did not turn up at all or came for follow up only once within 3 months after receiving treatment were also excluded from the study.
Seizure remission: When the seizure was totally or almost totally stopped it was labeled as ‘completely controlled’. If it was not totally controlled but was much improved by reduction of the frequency of seizure to half or more it was labeled as ‘much controlled’; and if the seizure remission was less than that, then it was leveled as ‘not controlled’.
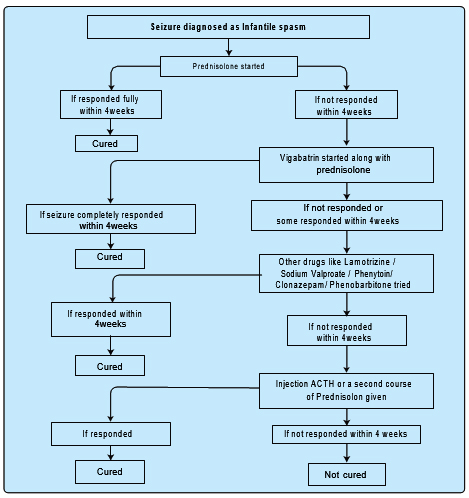
Treatment pattern: In each child, oral prednisolone was started initially in the dose of 2mg/kg and the drug was continued for at least 4-6 weeks and then gradually tapered off over a period of another 4-6 weeks time (figure 1). If seizure was not controlled with prednisolone within 4 weeks then the patient was switched over either to vigabatrin if the family could afford or to sodium valproate or benzodiazepine and prednisolone was tapered off. If seizure was not controlled with these drugs within 4weeks, injection ACTH was given for a period of 7-8 weeks if the family could afford. ACTH was given in a dose of 60iu/day for 3-4weeks, then the same dose was continued in alternate day for another 2 weeks and then at two days interval for another 2 weeks. If the child responded to prednisolone initially but seizure recurred after it was stopped then a second course of prednisolone was given in several cases. In intractable cases other drugs like benzodiazepine, phenytoin, phenobarbitone, lamotrizine were also tried one after one or in combination. (Figure 1).
Usually the family was requested to come for the first follow up at 4weeks and then after 2weeks of stoppage of prednisolone. Thereafter the follow up was given at regular interval but the time interval depended on the frequency of seizure, on other associated co-morbid conditions and on family’s intent.
Relevant investigations were usually done if the family could afford. Mostly EEG and USG of brain were done if the fontanels were open at the first visit. Then CT scan or MRI of brain was done if the child did not develop neuro-developmentally as expected after a couple of months. If the disability was severe in that case, these costly investigations were done earlier if the family could afford.
Results
A total of 110 children were studied. Male babies were 77(70.0%) and females were 33(30.0%). The male:female was 2.3:1. Of the total population, 62 (56.4%) was from urban and 48 (43.6%) were from rural areas. Mean age of first examination was 10.9 months and mean age at last follow up was 2.1 years (table I), 19 (17.3%) of the children had very early onset of seizure and majority, i.e. 76 (69.1%) developed their seizure within 3m to 1 year (table II).
|
Age at first visit |
Number (n) |
Percentage |
Age at last visit |
Number (n) |
Percentage |
|---|---|---|---|---|---|
|
Within 6months |
30 |
27.3 |
Up to 1 year |
16 |
14.5 |
|
> 6 months to 1 year |
54 |
49.1 |
> 1 yr to 2 yr |
41 |
37.3 |
|
>1 year |
26 |
23.6 |
> 2yr to 3 yr |
31 |
28.2 |
|
|
|
|
> 3yr |
16 |
14.5 |
|
|
|
|
> 4yrs |
6 |
5.5 |
|
Total |
110 |
100 |
Total |
110 |
100 |
Out of total, 74 (67.3%) of the children had associated motor developmental delay and 54(49.1%) had other associated problems, like crying, less responds, vision problem etc. In the antenatal period, 62 (56.4%) of the mother had no obvious illness. 13 (11.8%) had hypertension, four (3.6%) had gestational diabetes and 39 (35.5%) had associated other problems like oedema, pain, mild per vaginal bleeding and others.
|
Age of onset of seizure |
Number (n) |
Percentage |
|---|---|---|
|
Within 3 months |
19 |
17.3 |
|
> 3m to 6 months |
44 |
40 |
|
> 6m to 1 year |
32 |
29.1 |
|
> 1 year |
5 |
4.5 |
|
Could not mention |
10 |
9.1 |
|
Total |
110 |
100 |
In the natal period 93(84.5%) babies were full term and 17(15.5%) were preterm. 48 (43.6%) of the babies was born by cesarean section due to various reasons. 33(30.0%) of the children had history of severe birth asphyxia. In the postnatal period 40(36.4%) children had no problem. 40(36.4%) had neonatal seizure, 10(9.1%) had neonatal jaundice requiring management, 12(10.9%) had respiratory problem, two(1.8%) suffered meningitis, while 30(27.3%) had associated other problem in addition to seizure. Out of 110 children, 80 (72.7%) had seizure ‘completely controlled’ and in nin (8.2%) seizure was ‘much controlled’ with treatment. But in 21(19.1%) cases the seizure was ‘not controlled’ or ‘poorly controlled’ (table III).
|
Seizure control |
Number (n) |
Percentage |
|---|---|---|
|
Controlled |
80 |
72.7 |
|
Much controlled |
9 |
8.2 |
|
Not or poorly controlled |
17 |
15.5 |
|
Responded but recurred |
4 |
3.6 |
|
Total |
110 |
100 |
IS was controlled with prednisolone in 40 (36.4%) cases and prednisolone with other drugs in six(5.5%). ACTH was tried in 17(15.5%) children. Of these in five(4.5%) cases seizure was completely cured. In 21 (19.1%) cases seizure was controlled with vigabatrin alone (table IV). Vigabatrin was tried in 32 (29.1%) babies. Seizure was controlled in 80 (72.7%) cases. Oral Prednisolone alone controlled infantile spasm in 40 (36.4%) of children and another 6 (5.5%) cases along with other drugs.
|
Drug used to control seizure (n) |
Number |
Percentage |
|
|---|---|---|---|
|
Prednisolone |
40 |
36.4 |
|
|
ACTH |
5 |
4.5 |
|
|
Vigabatrin |
21 |
19.1 |
|
|
Clonazepam |
2 |
1.8 |
|
|
Nitrazepam |
1 |
0.9 |
|
|
Combination |
5 |
4.5 |
|
|
Prednisolone in combination |
6 |
5.5 |
|
|
with other drugs |
|
|
|
|
Total |
80 |
72.7 |
|
Discussion
In infantile spasm boys are more affected than girls. Male female ratio varies from 1.1:1 to about 2.8:1 in several large studies.1,13 Ninety percent of infantile spasms begin in those younger than 12 months. Peak onset is at age 4-6 months.2 In this study, a total of 110 babies were enrolled. Of this male: female was 2.3:1. 62 (56.4%) babies were from urban and 48 (43.6%) from rural areas. In our country, most of the studies showed male predominance. This gender difference may be due to discrimination. In this series 76 (69.1%) babies developed seizure before 1yr of age and only five (4.5%) developed the symptom after 1year of age. 19 (17.3%) had very early onset seizure (before 3months). In 44 (40.0%) cases the seizure appeared between 3-6months of age. In ten (9.1%) cases parents could not mention the exact age of onset of seizure.
In 70-75% cases, infantile spasms is usually of symptomatic variety. The proportion of cryptogenic cases varies from 8-42%. The percentage of idiopathic cases reportedly is 9-14%.7,15,16 Patients with symptomatic infantile spasms have an identified underlying neurological disorder that directly causes the spasms. The number of neurological diseases that can result in spasms is enormous, but some of the major categories include intrauterine insults and infections, hypoxic-ischaemic encephalopathy, malformations of cortical development, metabolic disorders, other genetic or chromosomal defects, meningitis, tumors, and neuro-cutaneous syndromes.17
Buruina et al found in their study of total 77 children, 10 (12%) had idiopathic IS, the remaining 67 cases (88%) being symptomatic. The most frequent aetiological factors found in the studied patients were cerebral malformations (including especially tuberous sclerosis) and perinatal hypoxic-ischaemic encephalopathy.18
In our study, 48 (43.6 %) had history of some form of maternal illness during the prenatal period. 33 (30.0%) of the babies suffered severe perinatal asphyxia. In the postnatal period 40(36.4%) had neonatal seizure either as a consequences of HIE or due to other reasons. 10(9.1%) had jaundice, 12 (10.9%) had respiratory problem, two (1.8%) had meningitis and 27 (24.5%) had other minor problems. So, 55 (50.0%) had some major problem during the postnatal period. Depending on this finding probably 35-50% was in
the group of symptomatic variety. But from neuro- developmental examination it was near about 67%. Again CT scan or MRI of brain was done only in 44 (40.0%) cases; of which 38 (34.5%) shows either damage or other findings like ventricular prominence or atrophy. With further investigations only it can be then concluded whether they would be in the symptomatic or in other groups.
Due to financial constraints investigations like EEG, CT scan or MRI of brain could not be done in each and every case. Mostly EEG was done in 84 (76.4%) cases. Presence of a hypsarrhythmia in EEG confirms the diagnosis of infantile spasms. EEG patterns may evolve over a period; they initially appear in the sleep EEG record and subsequently present during the awake state. Hypsarrhythmia is seen in 75% of patients with West.19 Here 60 (54.5%) showed characteristic EEG findings of Infantile spasm, in 18 (16.4%) cases other findings are found. In Six (5.5%) case EEG was normal. This may be due to the fact that all these babies came within a short period after the onset of seizure.
Studies show ACTH or prednisolone induces a reduction or complete cessation of spasms, as well as an improvement in the EEG, in approximately 50-75% of patients. Some patients who do not initially respond to ACTH may respond to prednisolone and vice-versa. While relapses occur in about one-third to one-half of patients, a second course of ACTH is often effective.16,19 Some studies, demonstrate that shorter time lag between diagnosis and treatment improves initial remission rate. Age of onset of the spasms has occasionally been correlated with treatment efficacy, with later onset (>8 months) having a better seizure control. Whether etiology of the infantile spasms influences responsiveness to treatment is also controversial.17
Among the conventional antiepileptic drugs, valproate and nitrazepam have been shown to be effective as first-line therapy in placebo-controlled clinical trials of spasms. Newer antiepileptic drugs, such as felbamate, lamotrigine, topiramate, and zonisamide have been tried with some success as adjunctive therapy in infantile spasms. Few studies have directly compared these other agents with hormonal therapy, making conclusions about relative efficacy difficult.
In this study, total remission of seizure occurred in 80 (72.7%) of the children. Of this 40 (36.4%) was controlled with prednisolone alone. Another six (5.5%) responded to prednisolone in combination of other drugs. ACTH was tried in 17 (15.5%) children. Of these five (4.5%) responded with ACTH. In three (2.7%) the spasm responded completely but recur again as ACTH was stopped. In five(4.5%) case no responds found. In others responds was variable. Vigabatrin alone controlled the spasm in 21 (19.1%) children. In 32 (29.1%) babies it was tried. Clonazepam or nitrazepam also brought remission in three (2.7%) cases. In five(4.5%) cases fit was controlled by combination of drugs other than Prednisolone or ACTH. In our country ACTH and Vigabatrin are very costly and also these are not easily available drugs. In addition to it injectable form of ACTH is difficult to continue outside the hospital. Difficulty to identify the visual field defect, which, may develop in children who gets vigabatrin also narrowed down its use. Also many of these children have associated loss of visual awareness or low vision during the period of spasm, this also make its use difficult.
In our experience, response to the cheaper drug prednisolone is so evident that we always use prednisolone as first choice of drug in the treatment of IS. Except weight gain there is no other major side effects seen during its use. In this study 36 (32.7%) responded to the first trial of prednisolone. In addition, another four (3.6%) cases responded to prednisolone when used for the second time as valproate, benzodiazepine or vigabatrin failed after the use of prednisolone initially. Also six (5.5%) responded to combination of prednisolone and other drugs. So, 46 (41.8%) children responded to prednisolone and in addition to it 19 (17.3%) had shown much remission in seizure.
Conclusion
Oral prednisolone, a cheaper drug, can thereby effectively be used as a first choice of drug for the control of infantile spasm. Vigabatrin is a good, but costly option for a drug in controlling Infantile spam.
Acknowledgments
Authors are very grateful to Professor Mozammel Hoque, Department of Biochemistry, BSMMU, for his critical review of the paper. Authors are also owe to Adib Sarwar eldest son of the principal author for his utmost co-operation in all aspects of writing of this paper.
References
- West WJ. A particular form of infantile convultions. Lancet. 1841; 1:724-25. Available From:
- Glauser TA, Morita DA, Stannard KM. Infantile spasm(West syndrome): eMedicine, Neurology. Last updated: 2010 April 26. Accessed 2010 November 2. Available From: http://emedicine.medscape..com/article/1176431-overview
- McQuarrie I, Anderson JA, Ziegler MR. Observation on the antagonistic effects of posterior pituitary and cortico- adrenal hormones in the epileptic subject. J Clin Endocrinol. 1942; 2: 406-10.. Available From:
- Hancock E, Osborne JP, Milner P. Treatment of infantile spasms (Cochrane Review). Last assessed as up-to-date: 2007 November 1. In: The Cochrane Library, Issue 4. Oxford: Update Software, 2002. Available From:
- Bobele GB, Bodensteiner JB. The treatment of infantile spasms by child neurologists. J Child Neurol. 1994; 9:432-5. Available From:
- Snead OC, III. Other antiepileptic drugs: adrenocorticotrophic hormone(ACTH). In: Levy R, Mattson R, Meldrum B, et al. eds. Antiepileptic drugs. New York: Raven Press. 1989:905- 12.. Available From:
- Riikonen R. A long-term follow-up study of 214 children with the syndrome of infantile spasms. Neuropediatrics. 1982; 13:14-23.. Available From:
- Riikonen R, Donner M. ACTH therapy in infantile spasms: side effects. Arch Dis Child. 1980;55:664–72.. Available From:
- Lombroso CT. A prospective study of infantile spasms. Clinical and therapeutic correlations. Epilepsia. 1983;24:135– 58.. Available From:
- Chadwick B. Comparison of monotherapy with valporate and other antiepileptic Drugs in the treatment of seizure disorders. Am J Med. 1988; 84:3-6.. Available From:
- Chiron C, Dulac O, Luna D. Vigabatrin in infantile spasm. Lancet. 1990; 335:363-64.. Available From:
- Sorel L, Dusaucy-Bauloye A. A pros de 21 case d’hypsarhythmia de Gibbs: Acta Neurologica Psychiatrica, Belgica. 1958; 58:130-41.. Available From:
- Aicardi J. Infantile spasm: Related syndromes. Epilepsy in children. 2nd edition, New York, Raven press, 1994: page 18-43.. Available From:
- Matsumoto A, Watanabe K, Negoro T, Sugiura M, Iwase K, Hara K, Miyazaki S. Long-term prognosis after infantile spasms: a statistical study of prognostic factors in 200 cases. Dev Med Child Neurol. 1981;23:51-65. Available From:
- Dulac O, Karen R, Ballaban-Gil, Solmon L.Moshe. West sydrome. Date update: 2005 April 28. Accessed 2010 November 7. available from http://www.ilae-epilepsy.org/ visitors/centre/ctf/west_syndrome.cfm. Available From:
- Wong M, Trevathan E. Infantile spasm. Paediatr Neurol 2001; 24:89-98. Available From:
- Buruiana F, Plesca D, Teleanu R, Davitoiu AM, Moiceanu M, Cretu L, Stefanescu M, Stancea I, Dragomir D. Etiological and neuroimagistic aspects in infantile spasms. Neuropediatrics. 2006; 37. Available From:
DOI: 10.1055/s-2006-94588 - Raj D Sheth. EEG in Common Epilepsy Syndromes: eMedicine Neurology. Last Updated: 2010 May, 20. Accessed 2010 November 10, available from http:// emedicine. medscape.com/article/113815-infantile spasm and west syndrome. Available From:
- Hrachovy RA, Frost JD, Kellaway PR, Zion TE. A double blind study of ACTH vs prednisolone therapy in infantile spasm. J Paediatr. 1983; 103: 641-5.. Available From:
Ex. Associate Professor, Child Development & Neurology unit, Dhaka Shishu Hospital, 1/1 B, Circular Road, Dhanmondi, Dhaka-1205, Bangladesh.
anisa.neuro@gmail.com
 0000-0003-2153
0000-0003-2153
Submission
14 November 2019
Accepted
17 October 2021
Published
01 December 2021
Apply citation style format of Bangladesh Medical Research Council
Issue
Vol 47 No 3 (2021)
Section
Research Articles
Financial Support
No fund was required
Conflict of Interest
Authors declare that they have no competing interests.