Murshed Ahamed Khan
Department of Endocrinology, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh.
Md Fariduddin
Department of Endocrinology, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh.
Mohammad Masum Alam
Department of Biochemistry, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, Bangladesh
Keywords: Parathyroid hormone, Vitamin D, Insulin resistance, Prediabetes
DOI: 10.3329/bmrcb.v47i3.59233
Abstract
Background: Several studies have found an inverse association among parathyroid hormone (PTH), vitamin D level, and insulin resistance (IR) causing prediabetes and diabetes.
Objective: To assess the level of vitamin D, PTH, and insulin resistance among adults with prediabetes and determine the association of PTH vitamin D and insulin resistance (IR).
Methods : This cross-sectional study was carried out in 140 newly detected adults with prediabetes according to ADA 2019 criteria. 25(OH) D cutoffs to define deficiency and insufficiency were used according to Endocrine Society (USA) criteria, Measurement of intact PTH, vitamin D and insulin (fasting) was done by chemiluminescent microparticle immunoassay (CMIA).
Results: In this study, most of the study population was 30 years and above (73.0%). The male-female ratio was 1:7, the majority of participants came from urban areas (81.0%). 37.0% had raised PTH and most of the participants (79.0%) were vitamin D deficient. A significant association was found between PTH and insulin resistance. Though it was observed that there was an increasing trend of insulin resistance across increasing severity of vitamin D deficiency but statistically it was not significant (p=0.74)
Conclusion: Our study results demonstrate an inverse relationship between PTH and insulin resistance but there was no association had been found between vitamin D and insulin resistance in individuals with newly detected untreated prediabetes. The clinical significance of these observations warrants further study to explore these relationships more appropriately.
Keywords: Parathyroid hormone, Vitamin D, Insulin resistance, Prediabetes.
Introduction
During the last decades, several studies indicate that there is a role of vitamin D as a biological metabolic regulator.1 Hypovitaminosis D seems to be implicated in the pathogenesis of prediabetes and diabetes and an inverse association between serum vitamin D and prediabetes prevalence has been reported.2
Prediabetes is an important glycaemic state that predisposes an individual to a high probability of future progression to diabetes and vitamin D deficiency is thought to influence the pathogenesis of type 2 DM by affecting either insulin sensitivity, a-cell function, or both.3,4 Activation of adipocytes modulates intracellular calcium concentrations and can affect changes in lipogenesis and lipolysis. It is therefore assumed that vitamin D is involved in modulating the tissue response to insulin.5 One of the hallmarks of type 2 DM is low-grade inflammation which can be a result of an increase in circulating cytokines such as tumor necrosis factor a (TNF-a) and interleukin (IL)-6 which contribute significantly to insulin resistance in muscle and adipose tissue.6 Vitamin D tends to down- regulate the transcription of various proinflammatory cytokine genes like IL-2, IL-12, and TNF-a.7,8
On the other hand, vitamin D and parathyroid hormone (PTH) are important physiological regulators of extracellular calcium homeostasis. Studies show that there is some biological plausibility for these relationships because low vitamin D levels and to a lesser extent elevated PTH levels have been associated with insulin resistance and glucose intolerance. 9-13
In insulin resistance, there is reduced glucose clearance in skeletal muscles, impaired suppression of glucose production by the liver, and decreased rates of lipolysis in adipose tissue or their combination. The longitudinal Whitehall II study described by Tabak et al found 29% lower insulin sensitivity at 13 years before the onset of T2DM.14 Thus IR represents an early abnormality that is compensated by augmented b- cell function for a long time before the insulin-glucose feedback loop fails.15
According to IDF atlas, the incidence and prevalence of prediabetes and diabetes are increasing progressively despite various preventive and therapeutic approaches adopted at government and NGO levels in our country. On the other hand, the level of vitamin D is low in most of the population, shown in different studies on Bangladeshi population.16,17
So, the objective of this study was to assess PTH, Vitamin D, and insulin resistance in newly detected untreated prediabetes adults in hospital and find out the cross-sectional associations of vitamin D and PTH levels with insulin resistance which may be of good help for the clinician to address the situation more appropriately.
Materials and Methods
This cross-sectional study was conducted in the department of endocrinology of Bangabandhu Sheikh Mujib Medical University (BSMMU) from March 2019 to February 2020. A total of 140 Adults (age group of 18yrs and above) with prediabetes according to ADA 2019 criteria, were enrolled in this study after getting ethical approval from the institutional review board (IRB) of BSMMU. Patients currently on vitamin D and calcium or who had received any one of them within the last 120 days and patients receiving any medications that may alter vitamin D level and glucose tolerance (anticonvulsant, ketoconazole, glucocor-ticoids, rifampicin, isoniazid, oral contraceptive) and patient having endocrine disorders (hyperthyroidism, hypothyroidism, hyperpara- thyroidism, cushing syndrome) or chronic disease like CKD, CLD were excluded from this study. Informed written consents were obtained from all subjects. Measurement of Intact PTH, vitamin D, and insulin (fasting) was done by chemiluminescent microparticle immunoassay (CMIA) in the department of biochemistry and molecular biology, Bangabandhu Sheikh Mujib Medical University (BSMMU). Insulin resistance was determined by the homeostasis model assessment of insulin resistance (HOMA-IR). The 25(OH) D cut-offs to define deficiency and insufficiency were used according to Endocrine Society (USA) criteria.18 Data were analysed using SPSS and presented as table and figure. p value ≤0.05 was considered as significant.Results
In this study, most of the population was 30 years and above (73.0%). Male female ratio was 1:7, majority of participant came from urban area (81.0%) most of them have an occupation that belonged to manual, unskilled, and unemployed, middle class was the main socio- economic category in the study population (table I).
|
Parameters |
Frequency% |
|---|---|
|
Age of the respondent |
|
|
Less than 30 years |
38 (27.1) |
|
30 years and above |
102 (72.9) |
|
Region |
|
|
Urban |
114 (81.4) |
|
Rural |
26 (18.6) |
|
Gender |
|
|
Male |
52 (37.1) |
|
Female |
88 (62.9) |
|
Occupation |
|
|
Managerial and professional |
24 (17.1) |
|
Nonmanual |
4 (2.9) |
|
Manual |
26 (18.6) |
|
unskilled |
6 (4.3) |
|
Institutionalized, retired, unemployed 80 (57.1) |
|
|
Socio- economic status |
|
|
Lower |
56(40) |
|
Middle |
65(46.4) |
|
Higher |
19(13.6) |
|
Physical Activity |
|
|
Low |
12 (9.1) |
|
Moderate |
116 (87.9) |
|
High |
4 (3.0) |
Within parentheses are percentages over column total Overweight and obese were (85.0%), most of the participants were vitamin D deficient group (79.0%) and insulin resistance present about 79.0% participants, 37.0% of the participants had raised PTH (table II)
|
Parameters |
Frequency (%) |
|---|---|
|
BMI |
|
|
Underweight & Normal |
20 (14.3) |
|
Overweight & Obese |
120 (85.7) |
|
Acanthosis nigricans |
|
|
Present |
6 (4.4) |
|
Absent |
132 (95.7) |
|
Vitamin D |
|
|
Deficiency (< 20 ng/ml) |
110 (78.6) |
|
Insufficiency (20-29.9) |
28 (20.0) |
|
Sufficiency (³30 ng/ml) |
2 (1.4) |
|
Insulin resistance |
|
|
IR absent (HOMA-IR < 2.6) |
30 (21.4) |
|
IR present (HOMA-IR ³2.6) |
110 (78.6) |
|
PTH |
|
|
Normal (18.5-88 pg/ml) |
88(62.8) |
|
Increased (> 88 pg/ml) |
52(37.1) |
|
Serum calcium corrected |
|
|
Normal(8.5-10.5mg/dl) |
132(98.6) |
|
Low (<8.5mg/dl) |
8 (5.7) |
Mathematically it was observed that there was an increasing trend of insulin resistance across increasing severity of vitamin D deficiency though it was not statistically significant (p=0.74). There was a significant association between PTH level and insulin resistance (p = 0.028), about 89% of the participant was insulin resistant among the increased PTH group while it was 73% among the normal PTH group. There was a significant association between physical activity and insulin resistance and those who were highly physically active had low insulin resistance (p<0.001). A significant association between BMI and insulin resistance (p=0.001) was found about 83.0% of participants with overweight and obese had insulin resistance. In this study, it was also found that gender has a significant association with insulin resistance (p<0.001) (table III).
|
Parameters |
|
HOMA IR status |
p |
|
|---|---|---|---|---|
|
(HOMA-IR < 2.6) |
(HOMA-IR ³2 .6) |
|||
|
Vitamin D status |
Deficiency (< 20 ng/ml) |
24 (21.8%) |
86 (78.2%) |
0.74 |
|
|
Insufficiency (20-29.9) |
6 (21.8%) |
22 (78.2%) |
|
|
|
Sufficiency (³ 30 ng/ml) |
0 |
2 (100%) |
|
|
Age of respondent |
Less than 30 years |
12 (31.6%) |
26 (68.4%) |
0.074 |
|
|
30 years and above |
18 (17.7%) |
84 (82.4%) |
|
|
Region |
Urban |
26 (22.8%) |
88 (77.2%) |
0.41 |
|
|
Rural |
4 (15.4%) |
22 (84.6%) |
|
|
Gender |
Male |
20 (38.5%) |
32 (61.5%) |
<0.001 |
|
|
Female |
10 (11.4%) |
78 (88.6%) |
|
|
Physical activity |
Low |
4 (33.3%) |
8 (66.7%) |
<0.001 |
|
|
Moderate |
22 (19.0%) |
94 (81.0%) |
|
|
|
High |
4 (100.0%) |
0 (0.0%) |
|
|
BMI |
Underweight & Normal |
10 (50.0%) |
10 (50.0%) |
0.001 |
|
|
Overweight & Obese |
20 (16.7%) |
100 (83.3%) |
|
|
PTH |
Normal (18.5-88 pg/ml) |
24 (27.3%) |
64 (72.7%) |
0.028 |
|
|
Increased (> 88 pg/ml) |
6 (11.5%) |
46 (88.5%) |
|
|
Serum Calcium |
Normal (8.5-10.5 mg/dl) |
30 (22.7%) |
102 (77.3%) |
0.128 |
|
(Corrected) |
Low (<8.5) |
0 (0.0%) |
8 (100.0%) |
|
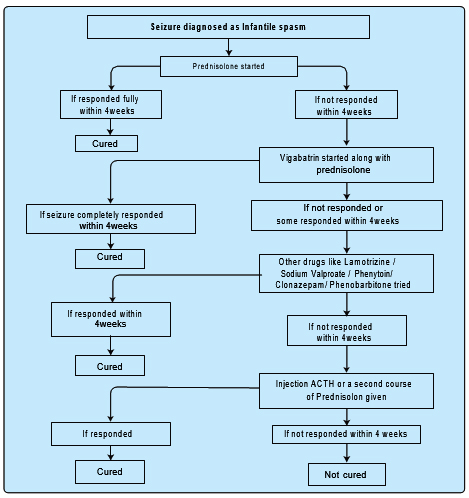
Distributions of PTH and insulin resistance among the participants were recorded (figure 1). This figure depicts that there was high insulin resistance among the high PTH group and there was a significant association between these two variables (p=0.028). (Figure 1).
The associations between insulin resistance with other co-factors were analysed by using an unadjusted and adjusted logistic regression model. The unadjusted model showed that female participants, BMI, overweight and obese group, and increased PTH group were positively correlated with insulin resistance. On the other hand, the vitamin D status of the participant had no role in insulin resistance. In the adjusted model we found that females were more likely to develop insulin resistance than males [OR 6.05, 95% CI (2.03 – 17.97)]. A similar kind of findings was also found in the overweight and obese group and increased PTH group where they were 2.36 and 2.58 times more prominent for developing insulin resistance than other counterparts (table IV).
|
Parameters |
Unadjusted OR |
p-value |
95% CI |
Adjusted OR |
p-value |
95% CI |
|---|---|---|---|---|---|---|
|
Vitamin D status |
|
|
|
|
|
|
|
Deficiency |
ref |
|
- |
ref |
|
- |
|
Insufficiency |
1.02 |
0.96 |
0.37 - 2.81 |
1.14 |
0.84 |
0.33 - 4.00 |
|
Sufficiency |
|
|
|
|
|
|
|
Age of the respondent |
|
|
|
|
|
|
|
Less than 30 years |
ref |
|
- |
ref |
|
- |
|
30 years and above |
2.15 |
0.078 |
0.91 - 5.505 |
1.28 |
0.67 |
0.39 - 4.22 |
|
Gender |
|
|
|
|
|
|
|
Male |
ref |
|
- |
ref |
|
- |
|
Female |
4.87 |
<0.001 |
2.05 - 11.56 |
6.05 |
0.001 |
2.03 - 17.97 |
|
Physical activity |
|
|
|
|
|
|
|
Low |
ref |
|
- |
ref |
|
- |
|
Moderate |
2.13 |
0.24 |
0.58 - 7.73 |
0.63 |
0.56 |
0.13 - 2.99 |
|
High |
|
|
|
|
|
|
|
BMI |
|
|
|
|
|
|
|
Underweight & Normal |
ref |
|
- |
ref |
|
- |
|
Overweight & Obese |
5.0 |
0.002 |
1.84 - 13.58 |
2.36 |
0.018 |
1.29 - 15.81 |
|
PTH |
|
|
|
|
|
|
|
Normal (18.5-88 pg/ml) |
ref |
|
- |
ref |
|
- |
|
Increased (> 88 pg/ml) |
2.87 |
0.033 |
1.08 - 7.59 |
2.58 |
0.01 |
1.66 - 41.29 |
Discussion
Vitamin D deficiency is a significant problem in this country as has been documented previously.16,17 Our study also showed that vitamin D insufficiency/ deficiency was common among individuals with prediabetes according to Endocrine Society criteria. In this study, it was found that there was no association between vitamin D and insulin resistance among adults with prediabetes. Similar findings were also observed in other studies done in people with prediabetes.22-24
There are different mechanisms for the effects of vitamin D on the pancreas: the presence of vitamin D receptors on pancreatic b cells, expression of vitamin D activating 1a hydroxylase in pancreatic b cells, the insulin gene having vitamin D response element, and the transcription of insulin receptor genes being increased by vitamin D. The protective role of vitamin D on prediabetes and diabetes, may be due to its well-known effects, such as its anti-inflammatory properties, its effects on calcium and phosphorus metabolism and regulation of the insulin receptor gene.25-27 It has been observed that vitamin D increases in calcium content of the cells, in turn leading to increased transport of glucose into the muscle.28
Vitamin D also regulates nuclear PPAR (Peroxisome proliferative activated receptor) that has an important role in insulin sensitivity.29 Vitamin D deficiency is associated with increases in inflammation. Vitamin D attenuates the expression of proinflammatory cytokines involved in insulin resistance such as IL-1, IL-6, TNF-a and also downregulates NF-Kb (Nuclear factor) activity.30
A review by Mitri et al found that people with higher vitamin D status (>25 ng/ml) had a decreased chance of getting glucose intolerance later in life compared to those with the lowest levels (<14 ng/ml).31 After conducting a meta-analysis and review of the impact of vitamin D and calcium on glycemic control in patients with type 2 diabetes, Pittas et al concluded that insufficient vitamin D and calcium appears to hinder glycemic control and that supplementing both nutrients may be necessary to optimize glucose metabolism in these patients.32 This study also found that female gender has an association with insulin resistance and similar findings also observed in another study in by Bhatt et al.33
The results of this study indicate that PTH status plays an important role in insulin resistance in the patient with prediabetes. The exact pathogenic mechanism between vitamin D/PTH and glucose intolerance is not yet understood. It has been suggested that PTH acts directly on b-cell or indirectly through augmentation of extracellular calcium intake and increase of peripheral insulin resistance.34 PTH increases cytosolic calcium in pancreatic cells and induces adipocyte tissue lipolysis in a dose- dependent manner through protein kinase A phosphorylation of the hormone-sensitive lipase (HLA) results in insulin resistance.35
Conclusion
The cross-sectional nature was one of the major limitations of our study. The present study had certain other limitations. Firstly, the number of study subjects, if higher, would have made the findings more significant. Secondly, the patients were from OPD of our hospital which was not a true representative of the normal population. Thirdly, presences of confounding effect of unforeseen variables (dietary habit, solar exposure etc.) that influence the variable parameters were not included in the present study). Fourthly, Liquid Chromatography-Tandem Mass Spectrometry (LC/MS) method was not available to measure vitamin D level. To summarise, vitamin-D deficiency/insufficiency is common among individuals with prediabetes in our country. However, this vitamin- D deficiency/insufficiency was not associated with insulin resistance in individuals with prediabetes. A significant association between PTH and insulin resistance has been found. Longitudinal prospective studies are warranted to assess whether this insulin resistance in prediabetes individuals with high PTH and lower vitamin D actually results in increased progression to prediabetes and diabetes in Bangladeshi adults.
Acknowledgments
The authors express their gratitude to to Bangabandhu Sheikh Mujib Medical University (BSMMU) authority for research grant and department of biochemistry & molecular biology, BSMMU for laboratory facilities. The authors also gratefully acknowledge department of endocrinology, BSMMU for technical support.References
- Muscogiuri G, Annweiler C, Duval G, Karras S, Tirabassi G, Salvio G, Balercia G, Kimball S, Kotsa K, Mascitelli L, Bhattoa HP, Colao A. Vitamin D and cardiovascular disease: from atherosclerosis to myocardial infarction and stroke. Int J Cardiol. 2017; 230: 577–84.
Doi:10.1016/j.ijcard.2016.12.053. - Grammatiki M, Rapti E, Karras S, Ajjan RA, Kotsa K. Vitamin D and diabetes mellitus: Causal or casual association? Rev Endocr Metab Disord. 2017;18:227-41.
Doi:10.1007/s11154-016-9403-y. - Deleskog A, Hilding A, Brismar K, Hamsten A, Efendic S, Östenson CG. Low serum 25-hydroxyvitamin D level predicts progression to type 2 diabetes in individuals with prediabetes but not with normal glucose tolerance. Diabetologia. 2012;55:1668-78.
Doi:10.1007/s00125-012-2529-x. - Chiu KC, Chu A, Go VL, Saad MF. Hypovitaminosis D is associated with insulin resistance and beta cell dysfunction. Am J Clin Nutr. 2004;79:820-25.
Doi:10.1093/ajcn/79.5.820 - Wallace IR, Wallace HJ, McKinley MC, Bell PM, Hunter SJ. Vitamin D and insulin resistance. Clin Endocrinol (Oxf). 2016: 84:159-71.
Doi:10.1111/cen.12760 - Hotamisligil GS, Arner P, Caro JF, Atkinson RL, Spiegelman BM. Increased adipose tissue expression of tumor necrosis factor-alpha in human obesity and insulin resistance. J Clin Invest. 1995;95: 2409-15
Doi:10.1172/JCI117936 - Schleithoff SS, Zittermann A, Tenderich G, Berthold HK, Stehle P, Koerfer R. Vitamin D supplementation improves cytokine profiles in patients with congestive heart failure: a double-blind, randomized, placebo-controlled trial. Am J Clin Nutr. 2006;83:754-59
Doi:10.1093/ajcn/83.4.754 - Pittas AG, Dawson-Hughes B. Vitamin D and diabetes. J Steroid Biochem Mol Biol. 2010 ;121: 425-29
Doi:10.1016/j.jsbmb.2010.03.042 - Chiu KC, Chu A, Go VL, Saad MF. Hypovitaminosis D is associated with insulin resistance and beta cell dysfunction. Am J Clin Nutr.2004; 79: 820-25.
Doi:10.1093/ajcn/79.5.820 - Chiu KC, Chuang LM, Lee NP, Ryu JM, McGullam JL, Tsai GP, Saad MF. Insulin sensitivity is inversely correlated with plasma intact parathyroid hormone level. Metabolism. 2000; 49: 1501-51
Doi:10.1053/meta.2000.17708 - Norman AW, Frankel JB, Heldt AM, Grodsky GM. Vitamin D deficiency inhibits pancreatic secretion of insulin. Science.1980; 209:823-25.
Doi:10.1126/science.6250216 - Liu E, Meigs JB, Pittas AG, McKeown NM, Economos CD, Booth SL, Jacques PF. Plasma 25-hydroxyvitamin d is associated with markers of the insulin resistant phenotype in nondiabetic adults. J Nutr. 2009;139: 329-34.
Doi:10.3945/jn.108.093831 - Forouhi NG, Luan J, Cooper A, Boucher BJ, Wareham NJ. Baseline serum 25-hydroxy vitamin d is predictive of future glycemic status and insulin resistance: the Medical Research Council Ely Prospective Study 1990-2000. Diabetes.2008; 57:2619-25
Doi:10.2337/db08-0593 - Tabak AG, Jokela M, Akbaraly TN, Brunner EJ, Kivimaki M, Witte DR. Trajectories of glycaemia, insulin sensitivity, and insulin secretion before diagnosis of type 2 diabetes: an analysis from the Whitehall II study. Lancet.2009; 373:2215-21.
Doi:10.1016/S0140-6736(09)60619-X
Assistant Professor, Department of Endocrinology, Room No.1520, Block-D, BSMMU, Shahbagh, Dhaka-1000, Bangladesh.
makhan1205@gmail.com
 0000-0002-2863-3867
0000-0002-2863-3867
Submission
01 November 2021
Accepted
25 November 2021
Published
01 December 2021
Apply citation style format of Bangladesh Medical Research Council
Issue
Vol 47 No 3 (2021)
Section
Research Articles
Financial Support
BSMMU, Dhaka
Conflict of Interest
The authors declared no potential conflicts of interest