Amit Roy Chowdhury
Department of Neurology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh.
M A Hannan
Department of Neurology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh.
Subash Kanti Dey
Department of Neurology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh.
Maftahul Jannat
Department of Neurology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh.
Md Habibur Rahman
Department of Neurology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh.
Keywords: Acute ischaemic stroke; Severity of stroke; Circle of Willis; NIHSS score.
DOI: 10.3329/bmrcb.v47i2.57778
Abstract
Background: The extent of damage by ischaemic stroke and the course of illness depend largely on the presence of collateral vessels around the affected area. The Circle of Willis (CoW), which serves as an important potential collateral pathway in maintaining adequate blood flow around the brain, is known to have variable patency. So the completeness of CoW is expected to influence the severity of ischaemic stroke.
Objective: The objective of the study was to determine the association of completeness of Circle of Willis with severity of acute ischaemic stroke.
Methods: It was a cross-sectional study done in Bangabandhu Sheikh Mujib Medical University, Dhaka from March, 2015 to August, 2017. A total of 42 patients of acute ischaemic stroke who were undergoing Digital Subtraction Angiography (DSA) for different reasons were selected by purposive sampling method. Data regarding completeness of Circle of Willis were obtained from DSA. National Institutes of Health Stroke Scale (NIHSS) score were measured to assess the severity of stroke. Then the severities of stroke between the complete and incomplete Circle of Willis groups were compared.
Results: A total of 27 male and 15 female patients were enrolled. Among them, 47.6% (20) had complete CoW and it was incomplete in rest 52.4% (22). Median (range) of NIHSS scores of complete and incomplete CoW group was 4.5 (0-17) and 9.5 (3-21) respectively. Mean NIHSS (±SD) for the complete and incomplete CoW was 6.60 (±4.97) and 9.95 (±5.10) respectively. The difference of mean between the two groups was found to be statistically significant (p=0.037). Odd’s Ratio (OR) for development of more severe stroke in patients with incomplete CoW was 4.5, 95% Confidence Interval (CI) 1.18-18.13 which was statistically significant (p=0.029).
Conclusion: It was concluded that incomplete Circle of Willis is associated with more severe stroke in acute ischaemic stroke patients.
Keywords: Acute ischaemic stroke; Severity of stroke; Circle of Willis; NIHSS score.
Introduction
Stroke is one of the leading causes of death in adult population throughout the world and is the most common cause of severe adult physical disability.1 It is now even a more increasing problem in all over the world. Increasing the portion of aging population and escalating risk factors such as hypertension, diabetes, tobacco abuse, unhealthy diet, obesity and physical inactivity may contribute to the recent pace of development of atherosclerosis and ultimately stroke.2
Ischemic Stroke constitutes about 85% of total stroke1 which occurs as a result of impaired blood supply to a certain area of brain. This impairment of blood flow can be compensated if adequate collateral blood supply could come in to assist. So the possibility of onset of stroke and the course of illness depends largely on presence of collateral vessels around brain.3 The Circle of Willis may act as an important potential collateral pathway in maintaining adequate cerebral blood flow in patients with such impairment of blood flow. It is formed by two internal carotid arteries and basilar artery anastomosing at the base of the brain. The size and patency of the arteries of the circle of Willis are known to be variable.4 The collateral potential of the Circle of Willis would be impaired if any component of this cycle is absent or hypoplastic.5 It is expected that that the anatomical variations of the Circle of Willis may affect the occurrence and severity of symptoms of such cerebrovascular accidents as infarctions.5
A lot of studies have already been done in different parts of the world about the variation and incompleteness of the Circle of Willis. But the relation between the incomplete Circle of Willis and the outcome or severity of stroke has not been much worked with. With the advances in micro-neurosurgery and endovascular procedures, we are getting more effective ability to deal with occlusive neurovascular diseases. So, the accurate knowledge of the intracranial vascular anatomy and its effect on disability and prognosis in ischemic stroke has become increasingly important. In this study, we investigated the relationship between incomplete Circle of Willis and severity of acute ischemic stroke.
Materials and Methods
This cross-sectional analytical study was conducted in Bangabandhu Sheikh Mujib Medical University, Dhaka from March, 2015 to August, 2017. Ethical approval was taken from the Institutional Review Board of the University. Many techniques are available to know about the configuration of Circle of Willis (CoW) including CT Angiogram (CTA), MR Angiogram (MRA) and Digital Subtraction Angiography (DSA). Though CTA and MRA are very sensitive, DSA is still considered to be the gold standard.6 To get the most accurate data about CoW, only DSA findings were considered in this study. Patients of acute ischaemic stroke who were undergoing DSA for various reasons were enrolled after written informed consent by purposive sampling method. As DSA is not very frequently needed in ischaemic stroke patients, only 42 patients could be enrolled. To measure the severity of stroke, National Institute of Health Stroke Scale (NIHSS) was used which is proved to be superior to other scales.7 NIHSS scores were measured within 7 to 15 days of stroke and all the data were recorded in a semi-structured case record form. Then the severity of stroke was correlated with completeness of Circle of Willis.
The results were expressed as means for continuous variables and as percentages for categorical variables. Mann-Whitney U test was done to compare the NIHSS of Complete and Incomplete CoW group. Significance of difference between the means of NIHSS was also tested by independent sample t-test. Samples were categorised into two groups to dichotomise the data by dividing the patients into groups of More Severe Stroke (consists of No signs of stroke and Minor Stoke groups) and Less Severe Stroke (consists of Moderate to Severe Stroke groups) based on NIHSS scoring. Association between Incomplete CoW and More Severe Stroke was tested by Chi-square test.
Results
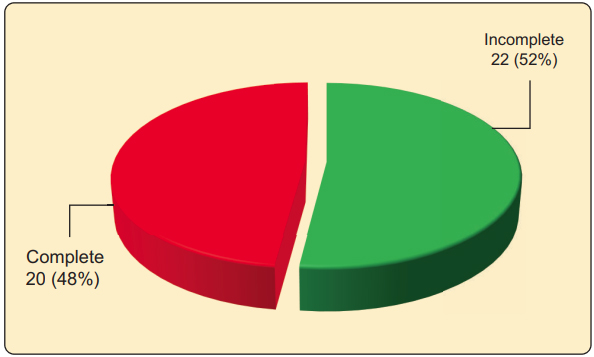
Out of total 42 patients, 15 (35.7%) patients were female and 27 (64.3%) were male.Among them, a majority of 52.4% of the patients had Incomplete Circle of Willis and the rest (47.6%) had it in Complete form (Figure 1).
NIHSS scores were compared in Complete and Incomplete Circle of Willis groups. It shows the median (range) for Complete and Incomplete group is 4.50 (0- 17) and 9.50 (3-21) respectively. The difference was found to be significant by Mann-Whitney U test (p=0.029).
The mean±SD of NIHSS was 9.95±5.103 for patients with Incomplete Circle of Willis was higher than the value 6.60±4.967 for patients with Complete Circle of Willis. The difference was tested with independent sample t test and it was found to be statistically significant (p=0.037, table I).
Completeness of Circle of Willis |
Mean NIHSS±SD |
p-value |
|---|---|---|
Complete Circle of Willis |
6.60±4.967 |
0.037 |
Incomplete Circle of Willis |
9.95±5.103 |
|
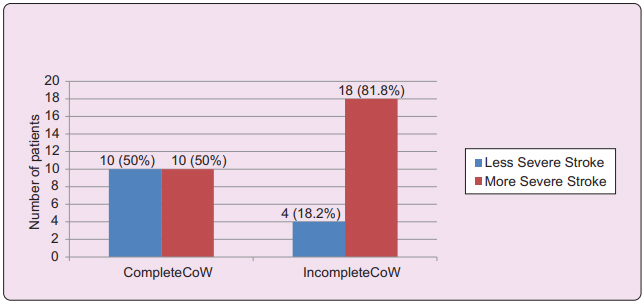
The data were dichotomised by dividing the patients into groups of More Severe Stroke and Less Severe Stroke. In patients with Complete Circle of Willis, 50% had Less Severe Stroke the rest 50% had More Severe Stroke. Patients with Incomplete Circle of Willis 18.2% patients had Less Severe Stroke the rest 81.8% had More Severe Stroke (Figure 2). The difference of severity between the groups was found to be significant (p=0.029) by Chi-square test.
The risk of development of more severe stroke was calculated for patients with Incomplete Circle of Willis. Here, Odd’s Ratio (OR) was 4.5. The lower and upper limit of 95% Confidence Interval of Odd’s Ratio were 1.18 and 18.13 respectively (p=0.029, table II).
Completeness of Circle of Willis |
Less Severe Stroke |
More Severe Stroke |
OR |
95% CI of OR |
p-value |
|
|---|---|---|---|---|---|---|
Lower |
Upper |
|||||
Incomplete |
4 |
18 |
4.5 |
1.18 |
18.13 |
0.029 |
Complete |
10 |
10 |
|
|
|
|
So, it is shown that risk of developing more severe stroke is higher in patients with Incomplete Circle of Willis. Positive correlation was found between Incomplete Circle of Willis with More severe stroke by Point Biserial correlation test (co-efficient, r= 0.322) which is statistically significant (p=0.037).
Discussion
This study was carried out with an aim to find out the association of incomplete Circle of Willis with severity of stroke in acute ischaemic stroke patients. The study findings were compared with result of some other published literatures elsewhere in the world. A total of 42 patients were enrolled in this study. The mean (± SD) age of the study population, was found to be 50 (±15.5) years ranging from 25-80 years. We found a male/female ratio of 1.8:1.
Circle of Willis was found to be incomplete in 52% patients and complete in the rest 48%. A similar study done in similar population by Iqbal in Kerala, India showed majority (52%) of the Circle of Willis were anomalous.8 In another study in Pakistani population, Siddiqi et al. found Circle of Willis was incomplete in 33.5% of individuals.9 Here we can see anomalies in Circle of Willis is very common in almost all the studies.
NIHSS score of the patients of acute ischemic stroke were compared between groups with complete and incomplete Circle of Willis. Mean (±SD) of NIHSS scores were 6.60 (±4.967) and 9.95 (±5.103) respectively for complete and incomplete Circle of Willis groups. The difference between the two groups was found to be statistically significant by unpaired sample t-test (p=0.037). Risk of development of More severe stroke in patients with Incomplete Circle of Willis was proved as the Odd’s Ratio (OR) was 4.5 and lower and upper limit of 95% confidence interval of Odd’s Ratio was 1.18 and 18.13 respectively. Our findings consisted with Zhou et al. in whose study the mean (±SD) of NIHSS score in complete and incomplete Circle of Willis group were found to be 5.65 (±5.15) and 7.45 (±5.27) respectively.10. The difference was strongly significant as p-value was 0.004. Chuang et al. also found similar results. Their median (range) NIHSS score for complete and incomplete CoW was 12 (8-18) and 17 (13-21) respectively.11 The difference was statistically significant, too (p=0.01). So, we can see that findings of different studies are similar to this study. Clearly, we can see that all of these above mentioned previous studies directly support findings of this study.
Conclusion
In this study, patients with incomplete Circle of Willis clearly showed a trend to develop more severe ischemic stroke in comparison with the patients with complete Circle of Willis. This trend is strongly supported by available data from limited number of previous studies. Further large scale studies should be carried out to reinforce the relation between incomplete Circle of Willis and severity of ischaemic stroke.
References
- Langhorne P. Stroke disease. In: Walker BR, Colledge NR, Ralston SH, Penmen ID, editors. Davidson’s Principle and Practice of Medicine. 22nd ed. Edinburgh: Elsevier; 2014. p. 1234-35.
- Das S, Chakrabarti K, Patnaek M, Roul L, Mohanti J, Sing SC. The Relationship of Carotid plaque, Intima Media Thickness (ITM), Resistivity Index (RI) and Pulsatility Index (PI) in Asian- Indian patients with Acute Ischemic Stroke with and without type DM. International Journal of Clinical Medicine. 2011; 2: 7.
- Smith WS, English JD, Johnston SC. Cerebrovascular disease. In: Hauser SH, Josephson SA, editors. Harrison’s Neurology in Clinical Practice. 3rd ed. China: McGraw-Hill Education; 2013. p. 256-98.
- Naveen SR, Bhat V, Karthik GA. Magnetic resonance angiographic evaluation of circle of Willis: A morphologic study in a tertiary hospital set up. Annals of Indian Academy of Neurology. 2015; 18: 391-97.
- Miralles M, Dolz JL, Cotillas J, Aldoma J, Santiso MA, Gimenez A. The role of the circle of Willis in carotid occlusion: Assessment with phase contrast MR angiography and transcranial duplex. European Journal of Vascular & Endovascular Surgery. 1995; 10: 424-30.
- Stock KW, Wetzel S, Kirsch E, Bongartz G, Steinbrich W, Radue EW. Anatomic evaluation of the circle of Willis: MR angiography versus intraarterial digital subtraction angiography. American Journal of Neuro Radiology. 1996;17: 1495-9.
- Young FB, Weir CJ, Lees KR. Comparison of the National Institutes of Health Stroke Scale with Disability Outcome. Measures in Acute Stroke Trials. Stroke. 2005; 36: 2187-92.
- Iqbal S. A Comprehensive Study of the Anatomical Variations of the Circle of Willis in Adult Human Brains. Journal of Clinical and Diagnostic Research. 2013;7: 2423-27.
- Siddiqi H, Tahir M, Lone KP. Variations in Cerebral Arterial Circle of Willis in Adult Pakistani Population. Journal of the College of Physicians and Surgeons Pakistan .2013; 23: 615-19.
- Zhou H, Sun J, Ji X, Lin J, Tang S, Zeng J, Fan Y. Correlation between the Integrity of the Circle of Willis and the Severity of Initial Noncardiac Cerebral Infarction and Clinical Prognosis. Medicine. 2016; 95: 2892.
- Chuang YM, Chan L, Lai YJ, Kuo KH, Chiou YH, Huang LW et al. Configuration of the Circle of Willis is associated with less symptomatic intracerebral hemorrhage in ischemic stroke patients treated with intravenous thrombolysis. Journal of Critical Care. 2013; 28: 166-72.
Department of Neurology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh.
dr.amit.roychowdhury@gmail.com
 0000-0001-8369-3372
0000-0001-8369-3372
Submission
05 August 2019
Accepted
01 December, 2019
Published
01 August 2021
Apply citation style format of Bangladesh Medical Research Council
Issue
Vol 47 No 2 (2021)
Section
Research Articles
Ethical Clearance
IRB of BSMMU, Dhaka, Bangladesh.
Financial Support
None
Conflict of Interest
There is no conflict of Interest.