Pran Gopal Datta
Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh.
Nasima Akhtar
Department of Otolaryngology-Head & Neck Surgery, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh.
Abirvab Naha
Department of Otolaryngology-Head & Neck Surgery, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh.
Anindita Datta
Department of Radiology and Imaging, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh.
Keywords: Schwannoma, Neurilemmoma, Schwann cell, Tonsil
DOI: 10.3329/bmrcb.v46i2.49025
Abstract
Background: Schwannoma is mostly benign lesion that originates from the Schwannoma cells that cover the myelinated nerve fibers. Schwannoma arising from the tonsil are very rare. In head and neck region the incidence rate of schwannoma is between 25 to 45%. In most of the cases vestibular nerve followed by a parapharyngeal space is involved. It is also known as neurilemmoma.
Objective: To diagnoses and manage the case of a Schwannoma of Tonsil.
Findings: A case of tonsillar schwannoma in a 42 years old males was reported. The patient presented with unilateral enlargement of left tonsil with congested pharyngeal mucosa.
Conclusion: Proper clinical examination with radiological assessment plays a vital role to diagnosis this accurately.
Keywords: Schwannoma, Neurilemmoma, Schwann cell, Tonsil.
Introduction
Schwannoma, also known as neurilemmoma, mostly benign lesion which originate in the ectodermal Schwann’s cell of the nerve fibers.1,2 This are relatively uncommon, slowly growing lesion and can arise throughout the body. 25 to 45% schwannoma have been reported to occur in head and neck region. In intraoral region, it is only 1%, where tongue is the most common site.3-6 But tonsillar schwannoma is very uncommon. It is very difficult to differentiate a schwannoma from other lesion of oral cavity by physical examination. A case of schwannoma which was clinically diagnosed as unilateral tonsillar hyperplasia suspected to be lymphoma, which caused obstructive symptoms with occasional sore throat in a middle aged male, has been reported here.
The Case
A 42 years old man from Chattogram, Bangladesh, presented in outpatient department of the Otolaryngology unit of Green Life Medical College & Hospital on 10th April, 2017 with chief complaints of repeated sore throat for last 6 years. He was married and father of two children. All of his family members were healthy. For last 5 months he experienced difficulty and pain during swallowing. On examination, it was to be found unilateral enlargement of left palatine tonsil with congested pharyngeal mucosa. On inspection, there was an oval shape mass with a smooth surface and pushing the left tonsil anteromedially with an extension up to supra-tonsillar region. It was measuring about (5X4) cm in size. On palpation, the surface was smooth, firm in consistency and non-tender. Other ENT examinations were unremarkable including neck palpation. After clinical examination, the provisional diagnosis was lymphoma and differential diagnosis was carcinoma of left tonsil.
Computed tomography (CT) of the head neck region revealed a well circumscribed and heterogeneous lesion in left oropharyngeal area (Figure 1).
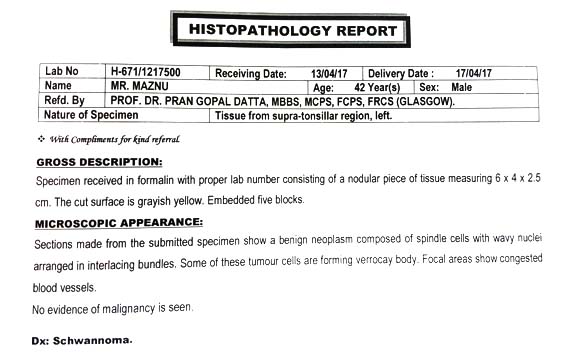
All relevant investigations were done and found within normal limit. After proper counselling and explanation, the entire left tonsil was excised under general anesthesia via trans-oral approach and specimen was sent for histopathological evaluation. Histopathology was suggestive of schwannoma (Figure 2)
The patient’s postoperative course was uneventful. On his follow-up we found the surgical field healthy and there was no evidence of infection or any residual tissue. After 1 month it was found complete healing of surgical area (Figure 3).
As it is mostly being in nature and in our case there was no evidence of malignant cell found in histopathology, the prognosis of it is very could and recurrence rate is very low. (Figure 4).
Discussion
In 1908, Verocay first described schwannoma or neurilemmona. They are mostly benign tumor which arises from schwann cell of nerve sheath which cover myelinated nerve fiber. The nerve sheath tumors which originate from peripheral nerves are of two types, Neurofibroma and Schwannoma. It can originate in any peripheral, autonomic or cranial nerve except the olfactory and optic nerve.7 About 25 to 45% of all schwannomas occur in the head and neck region.8 Only 1% cases may arise in oral cavity where tongue is the most common site but very rare in tonsil. Most of the case it may be mistaken for chronic tonsillar hyperplasia, malignant neoplasia, lymphoma, sarcoma or benign lesion like leiomyoma, lymphangioma, lipoma.9 To avoid such mistake, a detailed clinical history, physical examination, radiological and cytological assessment is essential.
Occurrence of schwannoma seen equal in both sexes at any age. Most often found in 2nd and 3rd decades of life and unlikely below 10 years of age.10 Parapharyngeal space is the most common site for schwannoma after vestibular schwannoma. A parapharyngeal space schwannoma may arise from IX, X, XI, XII and 3rd division of trigeminal nerve. Schwannoma arising from sympathetic chain or X, XI, XII nerve found in post styloid compartment and schwannoma of pre-styloid compartment mostly arise from lingual nerve, inferior alveolar nerve and auricular temporal nerve.11
Usually schwannomas are well encapsulated. For this reason it may passible to excise it with simple excision but recurrence may happen if the dissection is incomplete. In case of recurrence repeat excision is indicated. As schwannoma is radioresistance, radiotherapy is not indicated. During excision surgeon should do careful dissection to strip the nerve bundle from the tumor surface in order to preserve the nerve function.
In this case, computer tomographic findings of the mass were well circumscribed and encapsulated. We excised the left tonsil was extent on 13th April, 2017 and found a good surgical plane, that’s why complete removal of the tumor was done without any injury to tonsillar bed or vascular bundle of parapharyngeal space (figure 4). It believes that tonsillar schwannoma arise from glossopharyngeal nerve. However, in this case it didn’t observe any sign or symptom that could be attributable to damaged glossopharyngeal nerve.
Conclusion
Clinical examination along with imaging (MRI – more accurate) plays key role to make diagnosis of this rare condition accurately. For tonsillar schwannoma, surgical excision followed by histopathological confirmation is the choice of treatment. Though it is mostly being but it may be malignant also. So, histopathology must be done.
References
- Fawcett KJ, Dahlin DC. Neurilemmoma of bone. Am J Clin Path. 1967; 47: 759-66.
Doi:10.1093/ajcp/47.6.759 - Weiss SW, Goldblum JR. Benign tumors of peripheral nerve. Enzinger and Weissa: Soft Tissue Tumor (4th ed). 2001; 1111-207.
- Hatziotin JC, Aspirides H. Schwannoma of oral cavity. Oral surgery, Oral Med Oral Patho. 1967; 24:510-26.
- Das Gupta TK, Brasfield RD, Strong EW, Hajdu SI. Benign solitary schwannoma cancer. 1969; 24: 355-66.
- Zachariades N. Schwannoma of oral cavity. J Oral Med. 1984; 39: 41-43.
- Pfeifle R, Baur DA, Paulino A, Helman J. schwannoma of tongue report of 2 cases. J Oral Maxillofac Surg. 2001; 59: 802-4.
- Chaudhari N, Gupta D, Natesh V. Schwannoma of palatine tonsil. Ear Nose Throat J. 2011; 90: E7-9.
- Lall G, Walsh R, Rowlands D, & Donaldson I. Schwannoma (neurilemmoma) of the tonsil. The Journal of Laryngology & Otology. 1999; 113: 585-586.
- Mahendra IK, Sunil D, Pramod D. Schwannoma of the tonsil. International Journal of Medical Journal of Medical and Health Research. 2015; 1: 10-11.
- Batsakis JG. Tumours of head and neck. Clinical & pathological consideration 2nd Ed Williams and Wilkin, Baltimore. 1979; 313-33.
Doi:10.1002/hed.2890030117 - Bildirici K, Cakli H, Kecik C. schwannoma of tonsil. Otolaryngology Head and Neck 2002; 126: 693-4.
Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh
prangopal@gmail.com
 0000-0002-7034-1797
0000-0002-7034-1797
Submission
2020-07-20
Accepted
2020-07-30
Published
2020-08-01
Apply citation style format of Bangladesh Medical Research Council
Issue
Vol 46 No 1 (2020)
Section
Research Articles
Financial Support
None
Conflict of Interest
None