Gazi Shamim Hassan
Department of Orthodontics, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh.
Tanzila Rafique
Department of Orthodontics, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh.
Ranjit Ghosh
Department of Orthodontics, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh.
Ashis Kumar Biswas
Department of Orthodontics, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh.
Hasan Abeedur Rahman
Department of Orthodontics, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh.
Keywords: Autistic children, Oral hygiene status, Gingivitis, Poor tongue coordination
DOI: 10.3329/bmrcb.v46i2.49017
Abstract
Background: The worldwide incidence of oral health among the autistic children has been found to be poor for various reasons. Risk of dental caries and gingivitis is expected to be higher in these patients due to improper brushing and flossing because of the difficulties of the trainers and parents encounter when they brush the children’s’ teeth. They tend to pouch food inside the mouth instead of swallowing it due to poor tongue coordination, thereby increasing the susceptibility to caries. Communication and behavioural problems pose the most significant challenges in providing oral care.
Objective: The purpose of this study was to examine the oral health status and dental needs of autistic children in Bangladesh.
Methods: This case control study was carried out among 2-13 years old children with special health-care needs. The study was conducted in the Department of Orthodontics of Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka from the period of August to December 2017. A total of 130 children having ASD and aged between 2 -13 years were taken as cases and 182 gender-matched healthy children were taken as control. Cases were taken from BSMMU and other two autism centres. Controls were taken from a neighborhood school. Oral lesions were evaluated using standard international diagnostic criteria. Association of food habits and oral hygiene status were assessed among the study subjects. Dental status was evaluated using DMFT/dmft index according to the World Health Organization oral health surveys. Gingival health status were assessed using the Oral hygiene index of Loe and Silness, while the papillary bleeding index were assessed by employing the papillary bleeding index of Miihleman to ascertain the oral hygiene status.
Results: The mean age was found 8.72±3.40 years in the case group and 10.26±1.36 years in control group. Chi square test showed significant associations with the participants’ consumption of having more soft foods, presence of papillary bleeding and presence of decayed teeth with their oral hygiene status.
Conclusion: As data regarding oral health among autistic children are not available presently in Bangladesh. So, it is difficult for comparison of children having disabilities with those of healthy group. For planning and providing effective dental health care services for the children with autistic disorders.Keywords: Autistic children, Oral hygiene status, Gingivitis, Poor tongue coordination
Introduction
Autism is defined as complex developmental disability that typically appears during the first 3 years of life and is the result of a neurological disorder that affects the normal functioning of the brain, impacting development in the areas of social interaction and communication skills.1 It has no cure.2 Autism spectrum, also known as autism spectrum disorder (ASD), is a range of mental disorders of the neurodevelopmental type. Individuals on the autistic spectrum often experience difficulties with social communication and interaction and may exhibit restricted, repetitive patterns of behavior, interests, or activities. Symptoms are typically recognised between one and two years of age.3 Autism is highly heritable, although the genetics of autism is complex. It is a neuro developmental condition characterised by the impairment in social interaction, impaired communication, and restricted, repetitive, or stereotyped behaviours in the accessibility of evaluation and diagnostic services for children.4
According to data from the CDC, ASD prevalence was significantly higher in boys (26.6 per 1,000) than in girls (6.6 per 1,000). The overall estimated ASD prevalence for Asian/Pacific Islander children was 13.5 per 1,000.5
The population with (ASD) presents with similar health problems as that of the typical population, but due to factors including poor dietary preferences; behaviors and specific aversions, this population is at a greater risk and more susceptible to developing chronic non-communicable oral health conditions. The increasing prevalence of ASD coupled with this population being highlighted as one those with the greatest disease burden, has ignited an interest in their oral health concerns, which coincides with one of the global oral health goals to promote oral health within this population group. Individuals with special needs may have great limitations in oral hygiene performance due to their potential motor, sensory, and intellectual disabilities.5-8 Such conditions may make the affected children more prone to oral diseases and complicate their dental care.8 These children also commonly have damaging oral habits such as bruxism, tongue thrusting, picking at the gingiva, and lip biting.8,9 Several studies have reported a higher prevalence of caries, gingivitis, and poorer oral hygiene in comparison with non-autistic individuals,10-14 while others reported no differences in oral health status between autistics and controls; in some cases, the prevalence of caries in children with autism may even be comparatively lower. Maintaining optimal oral and dental health in intellectually and/or physically challenged children is of utmost importance, as these children usually suffer from several associated general health problems in addition to their primary condition. Furthermore, earlier reports on this group of individuals in our environment show that they have high unmet needs, especially periodontal treatment needs.10-14
Poor dental health not only further compromises their general health but may also aggravate negative social interaction with these children.15 The special children need continuous dietary supervision and assistance in maintaining optimal oral hygiene due to their poor intellectual development and compromised neuromuscular coordination. It is contemplated that health care workers with good oral health knowledge and preventive practices would play a better role in maintaining optimal oral health in the special children under their care.
Several studies have reported a higher prevalence of caries, gingivitis, and poorer oral hygiene in comparison with non-autistic individuals.16Few studies over the past show a higher rate of oral diseases among the autistic patients. Lack of this important data is a serious limitation to oral health comparison of children with disabilities and healthy children. It is also important to understand the disease pattern of both male and female children with autistic disorder for planning and providing effective dental health care services. The purpose of this study was to examine the oral lesions and dental status of autistic children as compared to the non-autistic children in Bangladesh.
Materials and Methods
It was a case control study. The study was conducted in the Department of Orthodontics of Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka, from the period of August to December 2017. A total of 130 children having ASD, aged between 2-13 years were taken as cases from BSMMU and other two autism centers and 182 gender-matched healthy children were taken as control from a neighborhood school. Participants having facial anomalies or parental unwillingness to give the written consent were excluded from the study. Demographic information such as age and gender were obtained for each subject prior to examination. Participants’ histories regarding their food habits, tooth cleansing behavior, regular visit to dental surgeon were taken. Clinical examination were conducted for both groups in the respective schools using electrical overhead light, disposable mouth mirror, tweezers, dental explorer, gauze, and wooden tongue depressor. Oral lesions were evaluated using standard international diagnostic criteria. Dental status were evaluated employing the DMFT/dmft index according to the World Health Organization oral health surveys.17,18 Gingival health status were assessed using the Oral hygiene index of Loe and Silness, while the papillary bleeding index were assessed by employing the Papillary Bleeding Index of Miihleman to ascertain the oral hygiene status.19,20 The clinical findings were communicated to the parents/guardians and written referrals were given to dental clinics whenever it was necessary.
SPSS (SPSS Inc., Chicago, IL, USA) version 20.00 was used for data entry and analyses. Descriptive statistics were carried out to assess the distribution of age, sex and religion among the study participants. Associations between the two categorical data were seen by the Chi-square tests. Logistic regression analysis was employed to determine the contribution of gender, type of food, cleaning habit, papillary bleeding index of Miihleman, DMFT to dental status of autistic children. The study was ethically cleared by the National Research Ethics Committee of the Bangladesh Medical Research Council.
Results
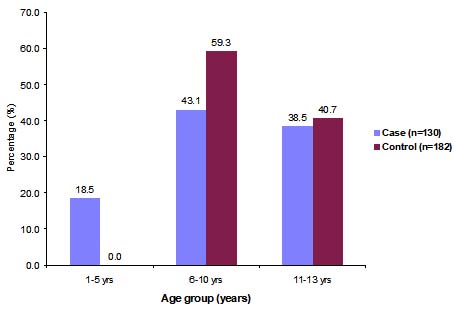
Regarding the age distributions of two groups, 56 (43.1%) and 108 (59.3%) participants were belong to the aged between 6-10 years in case and control group respectively. Next common age range were found between 11-13 years who comprised 50 (38.5%) of cases and 74 (40.7%) of control groups. Mean age in the case group was found 8.72±3.40 years and 10.26±1.36 years was found in control group (Figure 1).
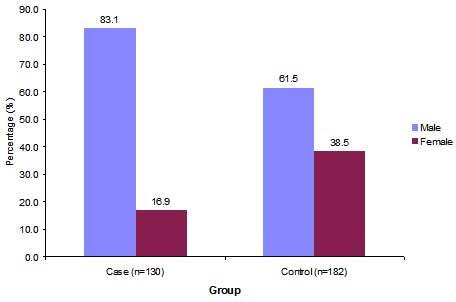
Among 312 school children, male respondents was 108 (83.1%) and 112 (61.5%) in case and control group respectively. Male children were predominant in both groups (Figure 2).
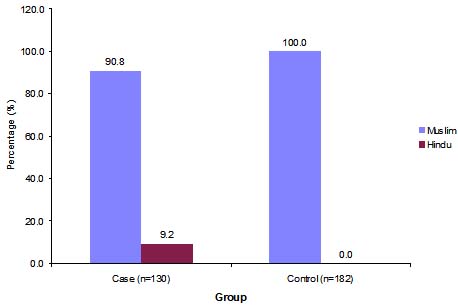
Among 312 school children, most of the respondents were Muslim in both groups. Only 12 (9.2%) respondents were found Hindu in the cases group. (Figure 3).
It was to be found that the significant value of p= <0.05 in mostly preferred foods by the participants’ and their oral hygiene practicing behavior (table I). The majority i.e. 98 (75.4%) of the children usually take food three times daily among the cases and 150 (82.4%) in control group respectively. Normal foods consumption rate as reported by the parents were found 100 (76.9%) among the case group children and 182 (100.0%) among control group children. The rest of the 28 (21.5%) among the case group were found to be consumed mainly soft drinks. Habits of taking more soft foods were found statistically higher in case group as compared to the control. About 56 (41.5%) participants were found to prefer the soft foods in case group and 114 (62.6%) mainly the carbohydrates in control group. In regards to the cleaning of teeth, 122 (93.8%) in case group and 182 (100%) in control group were known to clean teeth daily. Daily cleaning of teeth habit were found significantly higher in case group compared to the control.
| Variables | Case (n=130) No.(%) |
Control (n=182) No. %) |
P value |
|---|---|---|---|
| Food habits | |||
| How many times taken food | |||
| Twice daily Thrice daily More than three times daily No specific time |
10(7.7%) 98(75.4%) 20(15.4%) 2(1.5%) |
20(11.0%) 150(82.4%) 12(6.6%) 0(0.0%) |
0.178 |
| What type of food | |||
| Normal Soft foods Any consistency |
100(76.9%) 28(21.5%) 2(1.5%) |
182(100.0%) 0(0.0%) 0(0.0%) |
<0.001S |
| What type of food like best | |||
| Mainly Carbohydrate Mainly protein Mostly junk foods No Specific choice Soft food |
32(24.6%) 12(9.2%) 30(23.1%) 2(1.5%) 56(41.5%) |
114(62.6%) 10(5.5%) 46(25.3%) 8(4.4%) 4(2.2%) |
<0.001S |
| Oral hygiene practicing behavior | |||
| Does used to clean teeth daily Yes No |
122(93.8%) 8(6.2%) |
182(100.0%) 0(0.0%) |
0.017S |
| How often do brush teeth Once daily Twice daily More than twice daily |
62(50.8%) 54(44.3%) 6(4.9% |
90(49.5%) 86(47.3%) 6(3.3%) |
0.849 |
| What type of agent used to clean teeth Plane water Tooth brush and Paste Empty finger Tooth powder Other |
2(1.6%) 112(91.8%) 6(4.9%) 2(1.6%) 0(0.0%) |
0(0.0%) 168(92.3%) 2(1.1%) 8(4.4%) 4(2.2%) |
0.223 |
| At what time do used to clean teeth | |||
| In morning before taking breakfast | 56(45.9%) | 92(50.5%) | 0.085 |
| At bed time after taking dinner | 4(3.3%) | 0(0.0%) | |
| During taking bath | 2(1.6%) | 0(0.0%) | |
| In morning before taking breakfast + At bed time after taking dinner |
56(45.9%) | 76(41.8%) | |
| At bed time after taking dinner + In morning after taking breakfast |
4(3.3%) | 2(1.1%) | |
| In morning before taking breakfast + At bed time after taking dinner + In morning after taking breakfast |
0(0.0%) | 12(6.6%) | |
Chi-square test was performed to see the association between two groups
While considering the frequency of brushing teeth it was shown about once daily among 50.8% of case group and 59.5% among control group, twice daily among the 44.3% children in case group and 47.3% in the control group. Cleaning of teeth using tooth brush and paste were found 91.8% in case group and 92.3% in control group respectively. in case group, 45.9% children clean teeth in morning before taking breakfast and 45.9% both in the morning and at bet time after taking dinner, on the other hand 50.0% and 41.8% children in control group.
Data showed that 23.1% children among the cases and 22.0% children among the control used to visit the dental surgeon regularly. Purposes of visiting to dental surgeon for the extraction of tooth were found among 26.7% and 55.5% in case and control group respectively. Among 33.3% children the purpose of visit was for filling of decayed tooth in case group and 5.0% in control group. For other purposes visiting to dental surgeon were found 40.0% in case group and 40.0% in control group. No significant difference was found between two groups.
Presences of intra oral lesion were found in 2(1.5%) children and discolored tongues were found in 100% children of cases group.
The mean indexes of the oral hygiene were found 1.60±0.92 and 1.49±0.98 in case and control group respectively. There was no significant difference found between two groups.
The papillary bleeding index of Miihleman of the children showed the mean scores were 1.75±1.32 and 1.24±1.36 in case and control group respectively. Significant difference was found between two groups.
| Variables | Case (n=130) No.(%) |
Control (n=182) No. (%) |
p value |
|---|---|---|---|
| Visit to dental surgeon Yes No |
30(23.1%) 100(76.9%) |
40(22.0%) 142(78.0%) |
0.871 |
| Purpose of visit dental surgeon Extraction of tooth/teeth Filling of decayed tooth Other causes |
8(26.7%) 10(33.3%) 12(40.0%) |
22(55.0%) 2(5.0%) 16(40.0%) |
0.077 |
| Intra oral examination Oral lesion present Oral lesion absent |
2(1.5%) 128(98.5%) |
0(0.0%) 182(100.0%) |
0.093 |
| Type of lesion Apthous ulcer Traumatic ulcer Other (discolored tongue) |
0(0.0%) 0(0.0%) 2(100.0%) |
0(0.0%) 0(0.0%) 0(0.0%) |
- |
Chi-square test was performed to see the association between two groups
| Variables | Case (n=130) No. (%) |
Control (n=182) No. (%) |
p value |
|---|---|---|---|
| Oral hygiene index | |||
| No debris or stain present | 14(10.8%) | 28(15.4%) | 0.644 |
| Soft debris covering not more than one third of the tooth surface, or presence of extrinsic stains without other debris regardless of surface area covered. |
48(36.9%) | 72(39.6%) | |
| Soft debris covering more than one third, but not more than two thirds of the exposed tooth surface |
44(33.8%) | 46(25.3%) | |
| Soft debris covering more than two third of the exposed tooth surface |
24(18.5%) | 36(19.8%) | |
| Mean±SD | 1.60±0.92 | 1.49±0.98 | 0.497 |
| Papillary Bleeding Index of Miihleman | |||
| No bleeding | 22(16.9%) | 76(41.8%) | 0.003S |
| Only one bleeding point appearing | 42(32.3%) | 42(23.1%) | |
| Several isolated bleeding points or a small blood area appearing |
36(27.7%) | 26(14.3%) | |
| Interdental triangle filled with blood soon after probing |
6(4.6%) | 20(11.0%) | |
| Profuse bleeding when probing, spreads towards the marginal gingival |
24(18.5%) | 18(9.9%) | |
| Mean±SD | 1.75±1.32 | 1.24±1.36 | 0.020S |
Chi-square test was performed to see the association between two groups
The DMFT of the children showed that 40.0% of the children had decayed teeth in cases group and 57.1% in control group. Decayed teeth were found significantly more in control group. Dental carries was observed 100% children in cases group and 98.1% in control group.
| DMFT | Case (n=130) No. (%) |
Control (n=182) No. (%) |
p value |
|---|---|---|---|
| Presence of decayed teeth | 52(40.0%) | 104(57.1%) | 0.035S |
| Filled tooth with recurrent decay | 0(0.0%) | 2(1.9%) | |
| Dental caries | 52(100.0%) | 102(98.1%) | |
| Rampant | 2(3.8%) | 4(3.8%) | |
| Primary | 50(96.2%) | 100(96.2%) | |
| Presence of missing teeth | 14(10.8%) | 24(13.2%) | 0.649 |
| Causes of missing teeth Impaction Periodontal disease Un erupted teeth Gross caries |
6(42.98%) 2(14.3%) 2(14.3%) 4(28.6%) |
10(41.7%) 0(0.0%) 14(58.3%) 0(0.0%) |
|
| Filled tooth due to seal a root canal trauma | 2(1.5%) | 0(0.0%) | - |
Chi-square test was performed to see the association between two groups, s=significant
Table IV is showing the significant value of p = <0.05.
Primary dental caries were found 96.2% which was equal both in case and control group. Missing teeth were found 10.8% in case group and 13.2% in control group. Causes of missing teeth were 42.9% due to presence of impaction in cases group and 41.7% in control group. Unerupted teeth were found among 14.3% children of cases group and 58.3% among control group. Filled teeth following the root canal treatment due to the cause of trauma were found among 1.5% of case group children.
The results of logistic regression showed that all these variables like the male autistic children, habits of taking soft foods, presence of papillary bleeding and presence of decayed teeth were significant associated with oral hygiene status of the autistic children (table V).
| Variables | β | p-value | OR | 95% CI | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Sex (male) | 1.121 | 0.005 | 0.326 | 0.150 | 0.707 |
| Soft food | 2.086 | 0.002 | 8.052 | 2.208 | 29.36 |
| Bleeding | 1.527 | 0.006 | 4.606 | 1.542 | 13.75 |
| Presence of decayed | 0.693 | 0.036 | 2.00 | 1.047 | 3.820 |
The results of logistic regression showed that variables like male autistic children; habits of taking soft foods, presence of papillary bleeding and presence of decayed teeth are significantly associated with oral hygiene status of the autistic children.
| Variables | β | p value | OR | 95% C.I. for EXP(B) | |
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Food | |||||
| Soft | 1.541 | .055 | 0.21 | .044 | 1.03 |
| Normal food (R) | |||||
| Bleeding | |||||
| Yes | 0.854 | .075 | 0.43 | .166 | 1.09 |
| No (R) | |||||
| Presence of decayed tooth | |||||
| Yes | 0.733 | .090 | 2.1 | .892 | 4.86 |
| No (R) | |||||
| What Type of food you like best | |||||
| Mainly protein | 2.120 | .029 | 8.3 | 1.24 | 56.08 |
| Soft food | 3.931 | .004 | 50.9 | 3.51 | 741.02 |
| Other food (R) | |||||
Discussion
Maximum respondents 56 (43.1%) and 108 (59.3%) belonged to the age group of 6-10 years in case and control group respectively. Next common age ranged between 11-13 years were found 50 (38.5%) and 74 (40.7%) in case and control group respectively. Mean age of the participants in the case group were 8.72±3.40 years and 10.26±1.36 years in control group.
Out of the total children, male were found 108 (83.1%) among the cases and 112 (61.5%) among the control and male children were found predominant between the participants.
Food habits play an important role on person’s oral health. In this study, the majority of the children were found to take food daily three times 98 (75.4%) and 150 (82.4%) in case and control group respectively. Normal foods consumption by the children were reported by almost all of the parents in 100 (76.9%) and 182 (100%) of case and control groups. The rest of the 28 (21.5%) children belonged to the case group were reported to consume soft drinks.
Children with autism spectrum disorder (ASD) may have restrictive and ritualistic behaviors that affect their eating habits. Different children have different issues with food or refusing to eat one or more food groups or to eat certain textures (e.g. crunchy or soft). May getting hung up on particular flavours-often salty or sweet, which makes healthy eating much harder or may also needing either really strong or really bland food.21 Some studies also found many children with this disorder hold foods in their mouth but never swallow it, some have a condition called pica, in which they eat non-food items, such as dirt and paper. Some other behaviors reported in the study include smelling food before eating it.22
In this study, highest percentage was found among 56 (41.5%) of the participants in case group who prefer to intake soft foods more and in the control group 114 (62.6%) were found to prefer more carbohydrates based foods. In this study, significant association has been found between the preferred food habit and oral hygiene practice among the participants.
Frequency of brushing as contributing factors to caries levels in children with ASD has been found in many studies.23 In this study 122 (93.8%) children were reported in case group and 182 (100%) in control group to clean their teeth daily. Cleaning of teeth daily was found significantly higher in case group compared to the control. While assessing the frequency of teeth brushing it was found that 50.8% participants in case group and 59.5% participants in control group brush once daily and 44.3% children used to brush teeth twice daily in cases group and 47.3% in control group respectively. About 91.8% of the children belonged to the case group and 92.3% in control group clean the teeth by using tooth brush and paste as informed by their guardians. 45.9% of participants among the cases clean their teeth in morning before taking breakfast and 45.9% clean both morning and at bet time after taking dinner. On the other hand, it was found that in the control group 50.0% clean their teeth in morning before taking breakfast and 41.8% children clean both in the morning and at bet time after taking dinner. On the other hand, manual dexterity required for adequate tooth brushing resulting in poor and unsatisfactory plaque control and removal were also found in a study.24
Reviewing the responses of the participants regarding their visit to dental surgeon it was found that 23.1% and 22.0% children used to visit to dental surgeons in case and control groups respectively which contradicts the study findings in which lower frequency rate to visit to the dental surgeons were found by the ASD children due to presence of some barriers. Purposes of the visiting were known for the extractions of tooth were found among 26.7% of the cases and 55.5% among the control participants. 33.3% children were attended for filling of decayed tooth in case group and 5.0% in control group. For other causes visiting to dental surgeons were found among 40.0% of the participants in case group and 40.0% in control group. No significant differences were found between two groups.
Intra oral lesions were present in 2 (1.5%) children and 100% children had discolored tongue in case group.
While assessing the oral hygiene index of the children it was showed that mean hygiene index 1.60±0.92 and 1.49±0.98 in case and control group respectively. There was no significant difference found between the two groups.
Gingivitis is regarded as the most common periodontal disease in children, with the primary etiology as plaque. In poor oral hygiene food debris, plaque and micro-organisms also accumulate and the process of inflammation starts. This leads to gingivitis, which, if not taken care of can progress to gradual destruction of supporting soft and hard tissues of the teeth.18 This study revealed the presence of papillary bleeding index of Miihleman of the children with the mean score 1.75±1.32 and 1.24±1.36 in case and control groups respectively. Significant difference was found between the two groups which is almost similar with the study findings conducted in the Dubai and Sharjah Autism Centers where the gingival status evaluation the results showed that 97.0% (59/61) of the autistic children had gingivitis which is generalized in 78.0% of the examined children or localized in 22.0% of the cases.25
Missing teeth were found 10.8% in case group and 13.2% in control group. 42.9% missing of teeth were known due to the presence of impaction in cases group and 41.7% in control group. 14.3% missing teeth were found in case group and 58.3% in control group due to un erupted teeth. Filled tooth due to sealing of root canal followed by trauma was found in 1.5% respondents of case group.
Decayed teeth were found 40.0% of the children of case group and 57.1% in control group. Decayed teeth were found significantly more in control group. Though the prevalence of dental caries were found involving the one or more teeth of the 100% respondents in case group and 98.1% respondents in the control group but the primary caries were found 96.2% both in the case and control group. As the children with ASD were shown to prefer mostly soft type of foods so the susceptibility of the development of decayed teeth were found more in this group; this finding is related to the study conducted in Marmara University, Istanbul, Turkey.22 Additionally, the good supervision of the parents regarding tooth brushing probably an extremely large factor in children with ASD for having the same primary caries rate compare to those of the control group. Molars dominated the decayed component of the DMFT/dmft with an average caries prevalence of (51, 7% and 40, 8%) respectively were found in a study conducted in the KwaZulu-Nata, South Africa but the results displayed zero fillings indicative of unmet treatment needs.23 Missing teeth were presented in 10.8% participants in case group and 13.2% in control group. While assessing the causes of the missing of teeth it was found that 42.98% of missing teeth were due to presence of impaction in cases group and 41.7% in control group. 14.3% and 58.3% were caused by the unerupted teeth due to the age factor in case and control group respectively. Filled teeth with the root canal treatment followed by trauma were found in 1.5% of case group. In a study conducted in the Dubai and Sharjah Autism Centers where increasing in the number of missing and decayed teeth attributed to the effects of time on the increased number of teeth susceptible to decay such as the second permanent molars, which erupt during adolescent period.22
The multiple logistic regression analysis was employed to determine the contribution of the gender, types of food, teeth cleaning habit, presence of papillary bleeding index of Miihleman, DMFT to dental status of the autistic children. The results of logistic regression showed that all these variables were significantly related to oral hygiene practice. The association between male autistic children, habit of taking more soft foods, presence of papillary bleeding and decayed teeth are significantly associated with oral hygiene status of autistic children. Some other studies found another possible explanation for the presence of generalized gingivitis could be related to the side effects of medications. As the children with ASD increasing by the age, the number of caries is increasing; this finding is related to both the increasing number of permanent teeth and tooth brushing by family members becoming increasingly difficult with increasing age.23-25
Conclusion
Children with autism require special dental management to improve their oral health by maintaining efficient oral hygiene. An investigation in the peri-urban and rural areas is also need to be carried out. Attempts should be made by parents, general dentists and periodontists to teach oral hygiene methods to these patients by constant repetition and patience, as autistic individuals can develop skills over a period of time and lead a more productive and independent life.
Acknowledgments
We acknowledge with gratitude the financial support of the Research Grant Committee of BMRC, Dhaka, Bangladesh for the study. We are thankful to all participants for their cooperation and active participations. We are indebted to Prof. Dr. Shaheen Akhter, IPNA, BSMMU; Md. Mahbubul Munir, Generl secretary, SWID Bangladesh, (Dhanmondi branch); Creatitive Society for Children with Autism, Boro Mogbazar, Dhaka, Bangladesh and Taslima Akter, Head misterss, Dhanmondi 2 no. Prathomic Biddaloy for their whole hearted cooperation.
References
- Rutter M. Incidence of autism spectrum disorders: Changes over time and their meaning. Acta Paediatr. January 2007; 94:2-15.
- Barbaresi WJ, Katusic SK, Voigt RG. Autism: A review of the state of the science for pediatric primary health care clinicians. Arch Pediatr Adolesc Med. November 2006; 160:1167–75.
- Newschaffer CJ, Croen LA, Daniels J, Giarelli E, Grether JK, Levy SE, et al. The epidemiology of autism spectrum disorders. Annu Rev Public Health. April 2007; 28:235-258.
- Jaber MA. Dental caries experience, oral health status and treatment needs of dental patients with autism. J Appl Oral Sci. June 2011; 19:212–7.
- Geetha B.; Sugunadevi T.; Srija, B.; Laleethambika N.; Balachandar V. Art of Music, as Harmony of the Spheres and Autism Spectrum Disorder. Preprints 2016, 2016090022
Doi:10.20944/preprints201609.0022.v1 - Orellana LM, Silvestre FJ, Martínez-Sanchis S, Martínez-Mihi V, Bautista D. Oral manifestations in a group of adults with autism spectrum disorder. Med Oral Patol Oral Cir Bucal. May 2012; 17: 415-9.
- Al-Sufyani GA, Al-Maweri SA, Al-Ghashm AA, Al-Soneidar WA. Oral hygiene and gingival health status of children with Down syndrome in Yemen: A cross-sectional study. J IntSocPrev Community Dent. May 2014; 4:82-6.
- De Mattei R, Cuvo A, Maurizio S. Oral assessment of children with an autism spectrum disorder. J Dent Hyg. July 2007; 81: 65.
- Subramaniam P, Gupta M. Oral health status of autistic children in India. J ClinPediatr Dent. September 2011; 36:43-7.
- Desai M, Messer LB, Calache H. A study of the dental treatment needs of children with disabilities in Melbourne, Australia. Aust Dent J. 2001; 46:41–50.
- Vajawat M, Deepika PC. Comparative evaluation of oral hygiene practices and oral health status in autistic and normal individuals. J Int Soc Prev Community Dent. July –December 2012; 2:58–63.
- Vishnu Rekha C, Arangannal P, Shahed H. Oral health status of children with autistic disorder in Chennai. Eur Arch Paediatr Dent. June 2012; 13 9:126–31.
- Richa, Yashoda R, Puranik MP. Oral health status and parental perception of child Oral health related quality-of-life of children with autism in Bangalore, India. J Indian Soc Pedod Prev Dent. April 2014; 32:135-9.
- Waldman HB, Rader R, Perlman SP. Health related issues for individuals with special health care needs. Dental Clinic of North America. April 2009; 53:183–93.
- O'Brien G, Whitehouse AM. A psychiatric study of deviant eating behavior among mentally handicapped adults. Br J Psychiatry. August 1990; 157:281–4.
- Klein U, Nowak AJ. Characteristics of patients with autistic disorder presenting for dental treatment: A survey and chart review. Spec Care Dentist. March 1999; 19:200-7.
- Jaber MA, Sayyab M, Abu Fanas SH. Oral health status and dental needs of autistic children and young adults. J Investig Clin Dent. November 2010; 2:57–62.
- The American Academy of Periodontology. Proceedings of the World Workshop in Clinical Periodontics. Chicago: The American Academy of Periodontology; 1989: I/23-I/24.
- American Academy of Periodontology. Parameter on acute periodontal diseases. American Academy of Periodontology . J. Periodontol; May 2000: 863–6.
- Maweri S A, Ahmed W, Soneidar A, and Ghadah A. Sufyani A. Oral lesions and dental status of autistic children in Yemen: A case-control study. Journal of International Society of Preventive and Community Dentistry. December 2014; 4: 199-203.
- Dominguez-Rojas V, Astasio-Arbiza P, Ortega-Molina P, Gordillo-Florencio E, Garcio-Nunez JA, Boscones-Martinez A. Analysis of several risks factors involved in dental caries through multiple logistic regressions. Int Dent J. 1993; 43:149-56.
- Jaber MA. Dental caries experience, oral health status and treatment needs of dental patients with autism. J Appl Oral Sci. 2011; 19(3):212–7.
Doi:10.1590/s1678-77572011000300006 - Nath S. Feeding problems in children with autism. Interactive Autism Network at Kennedy Krieger Institute. Available From:www.kennedykrieger.org;2014.
- National Institute of Dental and Craniofacial Research. Epidemiology and oral disease prevention program. Oral health of United State children, the national survey of dental caries in U.S. school children: 1986-1987. Bethesda: NIDCR; 1989. (NIH Publication No. 89-2247)
- Lisa J. Heaton, Gavin M, BS, Peter M DDS, and Donald F. Downing, R P. Oral Health in Patients taking Psychotropic Medications: Results from a Pharmacy Based Pilot Study, PMC 2017 Jul 1. 56: 412–417.
Department of Orthodontics, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh
drgazishamim@yahoo.com
 0000-0001-8484-4080
0000-0001-8484-4080
Submission
2018-07-20
Accepted
2020-03-19
Published
2020-08-01
Apply citation style format of Bangladesh Medical Research Council
Issue
Vol 46 No 2 (2020)
Section
Research Articles
Financial Support
Bangladesh Medical Research Council (BMRC)
Conflict of Interest
There was no conflict of interest.