Namkha Dorji
Department of Obs & Gynae, Central regional referral hospital Bhutan.
Shirin Akter Begum
Department of Gynecological oncology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh.
Tasfia Mahmud
Ibrahim Medical College and BIRDEM Hospital, Dhaka, Bangladesh.
Mehriban Amatullah
Department of Gynecological oncology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh.
Keywords: VIA, Postcoital bleeding, Intermenstrual bleeding, Postmenopausal bleeding, Colposcopy, Histopathology
DOI: 10.3329/bmrcb.v46i1.47469
Abstract
Background: Cervical cancer is the most frequent cancer in women worldwide. It is a preventable and curable disease with proper screening. After primary screening Colposcopy is a valuable tool in the detection and treatment of precancerous cervical lesions. Histopathology is the gold standard method of diagnosis of Precancerous lesions.
Objective: The objective of this study was to evaluate the performance of colposcopy in the diagnosis and to make correlation between colposcopic & histopathological findings in precancerous cervical neoplasia (CIN).
Materials and Method: It was a cross sectional study, conducted at the Colposcopy Clinic, Bangabandhu Sheikh Mujib Medical University (BSMMU), Dhaka. Study was done for a period of one year from January, 2016 to December, 2016. Sixty two married women having following complaints: positive visual inspection of cervix (VIA + ve) with 3-5% Acetic acid, postcoital bleeding, postmenopausal bleeding, and intermenstrual bleeding were recruited for the study. Written informed consent was obtained from the participants. The questionnaire was pretested, corrected and finalized. The data collection was done using the interviewer administered questionnaire. Colposcopic examination of cervix was done in 62 participants. Colposcopy guided punch biopsy/Loop electrosurgical excision procedure (LEEP) from acetowhite area was taken in cases of VIA +ve women and random four quadrants (1, 5, 7 & 11 O’ clock position) cervical biopsy in cases of VIA – ve women having other indications. Histopathological examinations of specimens were done in the Department of Pathology, BSMMU. Descriptive analysis, chi-square test (X2) and Fisher’s exact test were performed. P value<0.05 was taken as statistically significant.
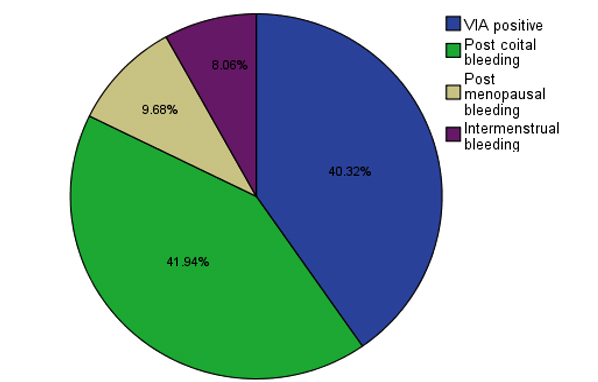
Result: The mean age of the study population was 36.8±11.9 years ranging from 20 to72 years. Out of 62 participants, 40.3% (n=25) had VIA positive, 41.9% (n=26) had postcoital bleeding among which 24 was VIA positive and 2 was VIA negative, 8.1% (n=5) had intermenstrual bleeding with positive VIA and 9.7% (n=6) post-menopausal bleeding among which 4 was VIA positive and 2 was VIA negative. Among total 62 participants
Sensitivity of colposcopy to diagnose histopathologically confirmed CIN I was 82.6%, CIN II was 25% and CIN III was also 25%. The specificity to diagnose CIN I was 42.4%, CIN II was 91.4% and CIN III was 93.1%. PPV of colposcopy to diagnose histologically confirmed CIN I was 55.8%, CIN II was 16.7% and CIN III was 20%. The NPV to diagnose CIN I was 73.7%, CIN II was 94.6% and CIN III was 94.7%. The colposcopic accuracy to diagnose CIN I was 61.3%, CIN II was 87.1% and CIN III was 90.3%. There was statistically significant (P value <0.05) correlation for colposcopic diagnosis of histopathologically confirmed CIN I,CIN II and III.
Conclusion:The accuracy of colposcopy to diagnose histopathologically confirmed precancerous cervical lesions was quite high. Patients presenting with postcoital bleeding and postmenopausal bleeding should have colposcopy and biopsies even if the screening test result normal. Moreover colposcopy has high sensitivity, so we can easily adopt the see and treat method to reduce the dropout.Keywords: VIA, Postcoital bleeding, Intermenstrual bleeding, Postmenopausal bleeding, Colposcopy, Histopathology
Introduction
Cervical cancer is most frequent cancer in women worldwide. In 2012, there was an estimated 5, 30,000 new cases. Every year, it causes estimated more than 2, 70,000 deaths. More than 85% of these deaths occur in less developed regions.1 In 2012, there was an estimated 4, 45,000 new cases in the less developed regions. Cervical cancer is second most common cancer among females of Bangladesh with an estimated 11,956 new cases and 6,582 deaths in 2012.2 In Bangladesh, cervical cancer is the most common reproductive cancer in women, and most women present when it is too late.3 Cervical cancer is responsible for the highest rate of mortality among Bangladeshi women.4 More than 80% of patients diagnosed with this eminently preventable cancer presents at clinically advanced and inoperable stages.5 As per the International Agency for Research on Cancer (IARC’s) projections for coming decades, deaths from cervical cancer will continue to rise.6
Cervical cancer is by far the most common HPV related disease. HPV 16 and 18 are responsible for 70% of precancerous cervical lesions and cervical cancer. Dr. Zur Hausen was awarded the Nobel Prize in Physiology or Medicine because of his pioneering work in demonstrating the role of HPV in cervical cancer on2008.7,8
Symptoms begin when the precancerous lesions become true cancer and invade surrounding tissues. The common symptoms include abnormal vaginal discharge which may be blood stained and foul smelling, post coital bleeding, postmenopausal bleeding, inter menstrual bleeding, excessive vaginal bleeding etc.Postcoital bleeding is regarded as a cardinal symptom of cervical cancer.9
As per USPSTF (United States Preventive Services Task Force) recommendation for cervical cancer screening: women aged 21 to 65 years are recommended to undergo screening with Papanicolaou smear every 3 years or, for those women between 30 to 65 years who want to lengthen their screening interval are recommended to screen with a combination of cytology and HPV testing every 5 years.10
National cervical cancer screening programme of Bangladesh was initiated in 2004 as a pilot study and as a national programme in 2005.3 In Bangladesh, government programme of screening test is VIA. Screening test is done in women aged at and above 30 years. There was good compliance for colposcopy but nearly half of patients with high grade precancerous lesions did not receive treatment. Cryotherapy use was infrequent and the policy of “see and treat” was rarely followed. Bangladesh is one of the first countries in the world to introduce VIA as the screening test for its national cervical cancer screening program.11
Conventional cervical cancer screening and prevention programmes require the woman to make at least two visits if the test is negative and frequent visits if the test is positive. However, the multiple visit based screening programmes has not been successful in reducing cancer rates in low resource settings. To improve the outcomes, unique single visit approach of “Screen and Treat” or “See and Treat” has been developed. A “See and treat” strategy minimises risk of loss of follow up though overtreatment may happened.12 There are studies that have demonstrated benefits of “see and treat” especially in low resource countries.13-15 VIA and cryotherapy were implemented for screening and treatment by the government partners at demonstration sites in Peru, Uganda and Vietnam. Evaluations in these three countries to explore barriers and facilitating factors showed that use of VIA and cryotherapy is a feasible approach in these settings for cervical cancer prevention services .13
The most important role of cervical cancer screening tests is to identify the woman with high grade squamous intra-epithelial lesions (HSIL) because the LSIL are frequently regressive.16
WHO expert panel recommended “screen and treat” strategies for patients with cervical intraepithelial lesions. The recommended screening methods are VIA alone, HPV test alone, HPV test followed by VIA and HPV test/cytology. The recommended treatment method is cryotherapy or LEEP. The expert panel did not recommend the use of cold knife conization (CKC) as treatment in a screen-and-treat strategy.17 There is no national guideline recommending either “see and treat” or “screen and treat” approaches in Bangladesh. However, Nessa et al.5 concluded that treatmentsshould be offered by cryotherapy or LEEP immediately following colposcopy at first visit instead of receiving treatment after confirmation by biopsy. Such an approach would benefit more women due to improved treatment compliance but it could also result in over treatment.
Materials and Methods
It was a cross sectional study, conducted at the Colposcopy Clinic, Bangabandhu Sheikh Mujib Medical University (BSMMU). Study was done for a period of one year from 1st January, 2016 to 31st December, 2016.Sampling technic was purposive sampling. All consecutive clients attending at colposcopy clinic BSMMU full filing inclusion criteria have been included. Sixty two married women having following complaints: positive visual inspection of cervix with 3-5% Acetic acid (VIA+ve), postcoital bleeding, postmenopausal bleeding, and intermenstrual bleeding were recruited for the study. Women having cervical growth, previously underwent treatment for precancerous lesion, pregnant women and women who didn’t give consent to participate in the study were excluded.Written informed consent was obtained from the participants. The questionnaire was pretested, corrected and finalized. The data collection was done using the interviewer administered questionnaire. Colposcopic examination of cervix was done in 62 participants. Colposcopic guided punch biopsy from acetowhite area were taken in cases of VIA +ve women and random four quadrants cervical biopsy was taken in cases of VIA – ve women having other indications. Histopathological examinations of specimens were done in the Department of Pathology, BSMMU. Descriptive analysis, chi-square test (X2) and Fisher’s exact test were performed. p value<0.05 was taken as statistically significant.
Results
The mean age (±SD) of the study population was 36.8±11.9 year ranging from 20 to72years. Maximum 71% (n=44) participants were in age range from 20 to 40 years. Regarding educational status 59.7% (n=37) participants had primary level education, 12.9% (n=8) were illiterate and remaining had SSC, HSC or higher degree. About their occupational status 90.3% (n=56) participants were house wives and others were employed. About socioeconomic status, 51.6% (n=32) of the study population were in the category of lower middle income group and 27.4% (n=17) were poor.
| Demographic characteristics | Frequency (n=62) | Percentage (%) |
|---|---|---|
| Age* (Years) | ||
| 20-30 | 22 | 35.5 |
| 31-40 | 22 | 35.5 |
| 41-50 | 11 | 17.7 |
| >51 | 7 | 11.3 |
| Education level | ||
| Illiterate | 8 | 12.9 |
| Primary | 37 | 59.7 |
| SSC | 8 | 12.9 |
| HSC | 4 | 6.5 |
| Graduate Occupation |
5 | 8.1 |
| House wife | 56 | 90.3 |
| Government service holder | 1 | 1.6 |
| Private service holder | 4 | 6.5 |
| Businesswoman Socioeconomic status |
1 | 1.6 |
| Poor | 17 | 27.4 |
| Lower middle | 32 | 51.6 |
| Upper middle | 12 | 19.4 |
| Rich | 1 | 1.6 |
| *Mean age ±SD (Range) | 36.8±11.9(20-72) |
About 96.8% (n=60) of the participants were sexually active and 3.2% (n=2) were widows. The mean age at marriage was 15.6±2.99 year ranging from 11 to 25 years. Among the studypopulation 61.3% (n=38) were married at the age of 10 to 15 years, 30.6% (n=19) at 16 to 20 years and the remaining 8.1% (n=5) at 21 to 25 years of age.
The mean age at first childbirth was 17.37± 2.98 years and ranging from 12 to 27 years. Regarding parity, 37.1% (n=23) were para 2 and others having para 3 or more.
Indication of colposcopy were 40.3% (n=25) due to VIA positive, 41.9% (n=26) postcoital bleeding, 8.1% (n=5) intermenstrual bleeding and 9.7% (n=6) post-menopausal bleeding.
| Colposcopic parameters | No. of cases (n=62) | Frequency (%) |
|---|---|---|
| Normal | 8 | 12.9% |
| CIN I | 43 | 69.4% |
| CIN II | 6 | 9.7% |
| CIN III | 5 | 8.1% |
| Total | 62 | 100% |
Colposcopic diagnosis of study population 12.9% (n=8) werenormal, 69.4% (n=43) wereCIN I, 9.7% (n=6) were CIN II and 8.1% (n=5) were CIN III.
| Histopathological parameters | No. of cases (n=62) | Percentage (%) |
|---|---|---|
| Chronic cervicitis | 19 | 30.6 |
| CIN I | 29 | 46.8% |
| CIN II | 4 | 6.5% |
| CIN III | 4 | 6.5% |
| CIS* | 3 | 4.8% |
| Cancer** | 3 | 4.8% |
| Total | 62 | 100% |
Regarding histopathological diagnosis, 30.6% (n=19) chroniccervicitis, 46.8% (n=29) CINI, 6.5% (n=4) CIN II, 6.5% (n=4) CINIII, 4.8% (n=3) carcinoma in situ and 4.8% (n=3) were invasive squamous cell carcinoma.
| Colposcopy | Histopathology | p value* | ||||||
|---|---|---|---|---|---|---|---|---|
| Total | Normal | CIN I | CIN II | CIN III | CIS | Cancer** | ||
| Normal | 8 | - |
4(50.0) | 1(12.5) | 3(37.5) | - |
- |
|
| CIN I | 43 | 17(39.5) | 24(53.8) | 2(4.7) | - |
- |
- |
0.000s |
| CIN II | 6 | 2(33.3) | - |
1(16.7) | - |
1(16.7) | 2(33.3) | |
| CIN III | 5 | - |
1(20.0) | - |
1(20.0) | 2(40.0) | 1(20.0) | |
| Histopathology | Total | p value* | ||||
|---|---|---|---|---|---|---|
| Positive | Negative | |||||
| Colposcopy | Positive | 24 | 19 | 43 | ||
| Negative | 5 | 14 | 19 | 0.032s | ||
| Total | 29 | 33 | 62 | |||
| Colposcopy | Positive | 1 | 5 | 6 | ||
| Negative | 3 | 53 | 56 | 0.284ns | ||
| Total | 4 | 58 | 62 | |||
| Colposcopy | Positive | 1 | 4 | 5 | ||
| Negative | 3 | 54 | 57 | 0.198ns | ||
| Total | 4 | 58 | 62 | |||
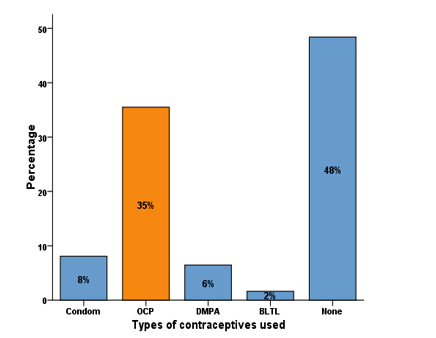
Regarding association of OCP useand precancerous and micro-invasive lesions, 35.5% (n=22) were OCPuserfor 5 to 10 years. Among them invasive squamous cell carcinoma of cervix were 13.63%% (n=3), Carcinoma in Situ were 4.54% (n=1), CIN III were 9.09% (n=2)andCIN I were 59.09% (n=13).Present study showed, significantassociation (p value 0.031) between the use of OCP and abnormal histopathology result.
Colposcopic diagnosis and histopathologic diagnosis of total 62 participants showed that 12.90% (n=8) participants with normal colposcopic finding. Though 12.90% (n=8)were colposcopically normal but histopathologically showed 50.0% (n=4) CIN I, 12.5% (n=1) CIN II and 37.5% (n=3) CINIII. Histopathologyreports of 69.35% (n=43) participants with CIN I on colposcopy, 39.5% (n=17) were normal, 53.8% (n=24) were CIN I and 4.7% (n=2) were CIN II.
Histopathology reports of 9.68 % (n=6) participants with CIN II on colposcopy, 33.3% (n=2) were normal, 16.7% (n=1) were CIN II, 16.7% (n=1) were CIS and 33.3% (n=2) were micro-invasive cancer.
Histopathology |
Total |
p value* |
|||
|---|---|---|---|---|---|
Yes |
No |
||||
| Colposcopy | Yes | 5 | 6 | 11 51 |
0.008s |
| No | 6 | 45 | |||
| Total | 11 | 51 | 62 | ||
| Strength of agreement between LSIL on colposcopy and LSIL on histopathology (n=62) | |||||
Histopathology |
Total |
p value* |
|||
Yes |
No |
||||
| Colposcopy | Yes | 24 |
19 |
43 | 0.032s |
| No | 5 |
14 |
19 | ||
| Total | 29 |
33 |
62 | ||
Histopathology reports of 8.06 % (n=5) participants with CIN III on colposcopy, 20% (n=1) were CIN I, 20% (n=1) were CIN III, 40% (n=2) wereCIS and 20% (n=1) were micro-invasive cancer (Figure 1).
The sensitivity, specificity, PPV, NPV and accuracy of colposcopy in diagnosing histopathologically confirmed CIN I were 82.6%, 42.4%, 55.8%,73.7% and 61.3% respectively. CIN II were 25.0%, 91.4%, 16.7%, 94.6% and 87.1% respectively. CIN III were 25%, 93.1%, 20%, 94.7% and 89% respectively.
The sensitivity, specificity, PPV, NPV and accuracy of Colposcopy in diagnosing HSIL were 45.5%, 88.2%, 45.5%, 88.2% and 80.6% respectively. There is a statistically significant (p value 0.008) association between colposcopy and histopathology to diagnose HSIL. Also Colposcopy in diagnosing LSIL were 82.8%, 48.8%, 55.8%, 73.7% and 61.3% respectively. There is statistically significant (p value 0.032) association between colposcopy and histopathology to diagnose LSIL (Figure 2).
Discussion
Cervical cancer is the fourth most common cancer in women worldwide (WHO, 2016).
In a study conducted by Parvin et al. 2016, the mean age of the study population was 37.57 ± 9.41 years, range from 20 to 60 years. The mean age of marriage of the study population was 16.33±3.35 years, range 10-30 years and mean age of delivery was 19.24±3.91 years, range 13-38 years.18
Present study showed the mean age of the study population was 36.8±11.9 years, range from 20-72 years. The mean age of marriage was 15.6±2.99 years, range 11-25 years. The mean age at first childbirth was 17.4 years and the mean parity was 2.8. The early age at marriage and early childbirth at young age and repeated pregnancies contributes to the risk of cervical cancer. All cases of invasive squamous cell carcinoma of cervix in present study was in age ranges of 31-50 years and were married at 15-17 years of age ranges.
In a study conducted by Rosenthal et al. 2001 in 314 women presenting with postcoital bleeding, 3% (n=9) had cervical cancer, 5% (n=17) had CIN I, 12% (n=37) had CIN II-III and rest of them having others disease. In the same study, the authors reported cervical cancer in 0.6% of women with postcoital bleeding who had normal looking cervices and normal smear.9
Present study showed 26 women with postcoital bleeding 16% (n=4) had normal, 60% (n=15) had CIN I, 8% (n=2) had CIN II, 4% (n=1) had CIN III, 3.8% (n=1) had CIS and 12% (n=3) had invasive squamous cell carcinoma of cervix on histopathology. Among 3 women diagnosed as cervical cancer with post coital bleeding, 3.8 % (n=1) of them presented normal looking cervices and normal smear.
Study by Boicea et al, 245 patients who presented with malignant findings at colposcopy and biopsy. Colposcopic findings in their study group: 11.4% (n=28) cases were CIN I, 20.4% (n=50) CIN II, 61.2% (n=150) CIN III, 5.3% (n=13) micro-invasive carcinoma and 1.6% (n=4) CIS. Histopathological results were: 1.6% (n=4) cases normal, 10.6% (n=26) CIN I, 22.4% (n=55) CIN II, 56.3% (n=138) CIN III, 6.1% (n=15) micro-invasive carcinoma and 2.8% (n=7) CIS. 19
Present study, out of 62 participants, colposcopy revealed 12.9% (n=8) normal and 87.1% (n=54) precancerous lesions. Histopathology revealed 30.6% (n=19) cases of chronic cervicitis, 46.8% (n=29) CIN I, 6.5% (n=4) CIN II, 6.5% (n=4) CIN III, 4.8% (n=3) carcinoma in situ and 4.8% (n=3) invasive squamous cell carcinoma. The differences in these studies, may be due to thedifferencesof sample size and expertise colposcopists.
Sensitivity of colposcopy compared to histopathology was 85.7% and specificity was 66.67% in a cross sectional study was carried out by Parvin et al, 2016.18
Present study showed.The sensitivity of colposcopy to diagnose LSIL and HSIL were 82.8% and 45.5% respectively and the specificity were 48.4% and 88.2% respectively.
Chaudhary et al. 2016 reported the PPV of colposcopy as 65.79%, NPV as 89.52% and accuracy as 80.5%. Present study revealed that the PPV of colposcopy to diagnose histologically confirmed CIN I was 55.8%, CIN II was 16.7% and CIN III was 20%. The NPV to diagnose CIN I was 73.7%, CIN II was 94.6% and CIN III was 94.7%. The colposcopic accuracy to diagnose CIN I was 61.3%, CIN II was 87.1% and CIN III was 90.3%.
Conclusion
In conclusion, the sensitivity and negative predictive value of colposcopy to diagnose LSIL were high but the specificity and positive predictive value were low. On the contrary, its specificity and negative predictive value to diagnose HSIL were high but sensitivity and positive predictive value were low. The accuracy of colposcopy to diagnose histopathologically confirmed precancerous cervical lesions was high.
In women presenting with postcoital bleeding and postmenopausal bleeding, cervical biopsy should be taken for histopathological confirmation, irrespective of colposcopic diagnosis. Endocervical curettage (ECC) should be done in women presenting with postmenopausal bleeding. Otherwise, significant numbers of highgrade lesions or invasive cancer will be missed if only colposcopy is considered.
References
- WHO, Fact Sheet, Human papillomavirus (HPV) and cervical cancer, June 2016. url: www.who.int/ mediacentre/factsheets/fs380/en/
Doi: - GLOBOCAN. Population Fact Sheet - Bangladesh GLOBOCAN 2012: Estimated Cancer Incidence, Mortality and Prevalence Worldwide in 2012.
Doi: - Ahmed T, Ashrafunnessa, Rahman J. Development of a visual inspection programme for cervical cancer prevention in Bangladesh. Reproductive health matters. 2008; 16:78-85.
Doi:10.1016/S0968-8080(08)32419-7 - Khatun S, Akram Hussain SM, Chowdhury S, Ferdous J, Hossain F, Begum SR, Jahan M, Tabassum S, Khatun S, Karim AF. Safety and immunogenicity profile of human papillomavirus-16/18 AS04 adjuvant cervical cancer vaccine: a randomized controlled trial in healthy adolescent girls of Bangladesh. Japanese journal of clinical oncology. 2011; 42:36-41.
Doi:10.1093/jjco/hyr173 - Nessa A, Hussain MA, Rahman JN, Rashid MH, Muwonge R, Sankaranarayanan R. Screening for cervical neoplasia in Bangladesh using visual inspection with acetic acid. International Journal of Gynecology & Obstetrics. 2010; 111:115-8.
Doi:10.1016/j.ijgo.2010.06.004 - Ferlay JS, Soerjomataram I, Ervik M, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F. GLOBOCAN 2012 v1. 0. Cancer incidence and mortality worldwide: IARC Cancer Base. 2013; 11.
Doi:10.1002/ijc.29210 - Zur Hausen H. Human papillomaviruses and their possible role in squamous cell carcinomas. Current topics in microbiology and immunology. 1977; 78:1-30.
Doi:10.1007/978-3-642-66800-5_1 - Zur Hausen H. The search for infectious causes of human cancers: where and why (Nobel lecture). Angewandte Chemie International Edition. 2009; 48:5798-808.
Doi:10.1016/j.virol.2009.06.001 - Rosenthal AN, Panoskaltsis T, Smith T, Soutter WP. The frequency of significant pathology in women attending a general gynaecological service for postcoital bleeding. BJOG: An International Journal of Obstetrics & Gynaecology. 2001; 108:103-6.
Doi:10.1111/j.1471-0528.2001.00008.x - Moyer VA. Screening for Cervical Cancer: U.S. Preventive Services Task Force Recommendation Statement. Annals of Internal Medicine [Internet]. American College of Physicians; 2012; 156:880.
Doi:10.7326/0003-4819-156-12-201206190-00424 - Basu P, Nessa A, Majid M, Rahman JN, Ahmed T. Evaluation of the National Cervical Cancer Screening Programme of Bangladesh and the formulation of quality assurance guidelines. BMJ Sexual & Reproductive Health. 2010; 36:131-4.
Doi:10.1783/147118910791749218 - Kuroki LM, Bergeron LM, Gao F, Thaker PH, Massad LS. See-and-Treat Loop Electrosurgical Excision Procedure for High-Grade Cervical Cytology: Are We Overtreating. Journal of lower genital tract disease. 2016; 20:247-51.
Doi:10.1097/LGT.0000000000000230 - Paul P, Winkler JL, Bartolini RM, Penny ME, Huong TT, Kumakech E, Mugisha E, Jeronimo J. Screen-and-treat approach to cervical cancer prevention using visual inspection with acetic acid and cryotherapy: experiences, perceptions, and beliefs from demonstration projects in Peru, Uganda, and Vietnam. The oncologist. 2013; 18:1278-84.
Doi:10.1634/theoncologist.2013-0253 - Denny L, Kuhn L, De Souza M, Pollack AE, Dupree W, Wright TC. Screen-and-treat approaches for cervical cancer prevention in low-resource settings: a randomized controlled trial. Jama. 2005; 294:2173-81.
Doi:10.1001/jama.294.17.2173 - Megevand E, Van WW, Knight B, Bloch B. Can cervical cancer be prevented by a see, screen, and treat program? A pilot study. American journal of obstetrics and gynecology. 1996; 174:923-8.
Doi:10.1016/S0002-9378(96)70327-7 - Advisory Committee on Cancer Prevention. Recommendations on cancer screening in the European Union. Eur J Cancer. 2000; 36:1473-8.
Doi: - World Health Organization. WHO guidelines for screening and treatment of precancerous lesions for cervical cancer prevention: supplemental material: GRADE evidence-to-recommendation tables and evidence profiles for each recommendation. World Health Organization; 2013. url: apps.who. int/iris/ bitstream/ handle/10665/ 96735/WHO_RHR_13.21_eng.pdf
Doi: - Parvin S, Kabir N, Lipe YS, Nasreen K, Alam KN. Correlation of pap smear and colposcopic finding of cervix with histopatholgiocal report in a group of patient attending in a tertiary hospital. Journal of Dhaka Medical College. 2013; 22:39-44.
Doi:10.3329/jdmc.v22i1.15604 - Boicea A, Patrascu A, Surlin V, Iliescu D, Schenker M, Chiutu L. Correlations between colposcopy and histologic results from colposcopically directed biopsy in cervical precancerous lesions. Rom J Morphol Embryol. 2012; 53:735-41. url: pdfs.semanticscholar.org/ ccfb/3e9116ef 88767 390cee5c047ca83bbeb2130.pdf
Doi:
Department of Gynaecological Oncology, Bangabandhu Sheikh Mujib Medical University, Dhaka, Bangladesh.
shirin.bsmmu@gmail.com
 0000-0001-5621-1390
0000-0001-5621-1390
Submission
2019-10-23
Accepted
2020-04-01
Published
2020-04-01
Apply citation style format of Bangladesh Medical Research Council
Issue
Vol 46 No 1 (2020)
Section
Research Articles
Financial Support
None
Conflict of Interest
Authors declare no conflict of interest